Post-Acute Traumatic Brain Injury Rehabilitation Treatment Variables: A Mixed Methods Study
Article information
Abstract
Purpose
This study explores gains in function, measured by the Mayo-Portland Adaptability Inventory-4 (MPAI-4) and qualitative interviews, of individuals who participated in a Post Hospital Interdisciplinary Brain Injury Rehabilitation – Residential (PHIDBIR-R) program as part of their recovery from brain injury.
Methods
The study uses a mixed methods design to identify correlates and explore pathways to functional recovery. Change scores from the MPAI-4 were derived to identify participants with greatest functional improvement. Qualitative interviews were employed to understand PHIDBIR-R program constructs associated with functional improvement. MPAI-4 data were derived from a bank of 135 PHIDBIR-R programs in 22 states. Participants were adults who sustained a brain injury and participated in a PHIDBIR-R program. 57 participants were identified as highest scorers; 10 completed semi-structured interviews.
Results
Data were analyzed using constant comparison procedures and rigorous credibility techniques. Thirteen themes within four categories (support, therapies, continuum of care, environment of care) emerged, reflecting participants’ understanding of constructs contributing to positive outcomes.
Conclusions
The results provided a cogent framework for program development, stakeholder program selection, and advocate and legislator considerations.
INTRODUCTION
Traumatic brain injury (TBI) is an alteration in brain function or other evidence of brain pathology caused by an external force. These injuries manifest as mild, moderate, or severe impairments to one or more areas, such as cognition, communication, memory, concentration, reasoning, physical functions, and psychosocial behavior [1].
The consequences of brain injuries are numerous with the potential to create life-long challenges for survivors and their families. Stories involving TBI permeate the news: the high-school athlete concussed in a football game, the soldier wounded in an explosive blast, and the teenager injured in a car accident. In these scenarios, futures transition from navigating routine activities to struggling to function.
A formidable fact surrounding these circumstances is that brain injury does not discriminate – it can happen to any person, at any time. Each year in the United States, 1.7 million TBIs occur either as an isolated injury or in conjunction with other injuries or illnesses. In the U.S., TBI is a contributing factor to nearly a third (30.5%) of all injury-related deaths [2] and figures indicate that 5.3 million people live with a TBI-related disability [3]. Annually, TBIs cost Americans $76.5 billion in medical care, rehabilitation, and loss of work [4,5].
Other etiologies of brain injury further elevate these numbers. The annual incidence of stroke is 795,000 [6]. Further, the annual estimate of brain tumors is 64,530, along with 27,000 aneurysms, and 20,000 viral encephalitis cases [6–8]. No national data are available for anoxic brain injury and other subtypes [1]. When all types of brain injury are aggregated, the annual occurrence in the U.S. approaches 8.5 million.
In addition, brain injuries reach beyond the individual who has sustained the TBI, affecting the lives of loved ones. Grief-stricken families witness trauma, entering a reality in which survival is the daily hope. Improvements in medical care have improved life expectancy, yielding a steady increase in the number of older adults living with a brain injury [9,10].
Once evident that an individual will survive the brain injury, goals focus on regaining lost function or rehabilitation. Just as each individual is unique, so is each recovery. Families commonly observe physical disabilities, impaired learning, and personality changes post injury. Nearly 20 years ago, the National Institutes of Health held a conference wherein an expert panel recommended that patients with TBI receive an individualized rehabilitation program based on the patient’s unique strengths and capacities, and adapted to needs over time. The group further advised that persons with moderate to severe brain injuries have individually tailored treatment programs that draw on the coordinated skills of various specialists [11].
Past research of rehabilitation following brain injury has often focused on the evaluation of a specific treatment modality or of a program’s efficacy as quantified by outcomes measurements. Many studies have sought to determine if rehabilitation has been successful, perhaps to the detriment of learning how rehabilitation has been efficacious. Studying how rehabilitation works over time is important in learning more about the individual and family experience while advancing an understanding of measured functional improvements.
Current research explores the therapies and interventions that facilitate long-term recovery of function. Individuals follow diverse recovery paths because there are a wide variety of options for rehabilitation [12]. This study focuses on Post-Hospital Inter-Disciplinary Brain Injury Rehabilitation – Residential (PHIDBIR-R) programs, which are 24-hour, 7-days a week rehabilitative care programs delivered in non-hospital, home-like, community-based environments. PHIDBIR-R programs strive to implement effective therapeutic interventions, supports, and services that maximize functional gains; these programs are judged on their ability to produce improvements in function [13].
While research efforts have focused on demonstrating positive outcomes, the identification of attributes that contribute to how improvement happens is largely untouched [13–18]. Although several PHIDBIR-R programs report positive outcomes [19,20], the empirical evidence is limited and studies habitually focus on quantitative analysis. Including a qualitative component may provide insight into the PHIDBIR-R, eludicating how these experiences advance an understanding of functional improvements.
METHODS
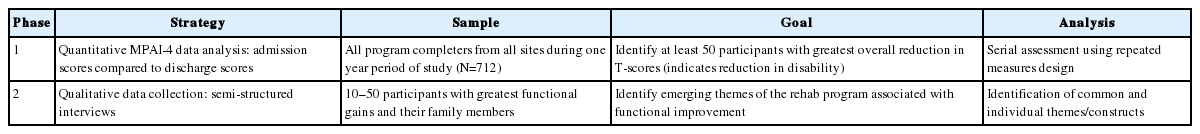
This study applied a mixed methods approach with two phases (Table 1). Phase 1, a participant selection variant [21], employed a quantitive approach to identify participants for Phase 2, which entailed qualitative inquiry. Participants were selected from a convenience sample from a large neurehabilitation company with more than 25 PHIDBIR-R programs nationally. Human subjects approval was secured through an accredited university’s Institutional Review Board (Protocol # 14-0298).
A repeated measures design was used in Phase 1 to compare scores of the Mayo-Portland Adaptability Inventory-4 (MPAI-4) [22] at admission and at discharge (n=712). Calculating difference in T-scores, all eligible participants were rank ordered and assigned to one of four categories of highest to lowest achievement. Additional analyses were completed to ascertain 1) which parts of the MPAI-4 showed statistically significant change (paired t-tests); and 2) which of the 29 items contributed most to change scores (MANOVA).
Phase 1 identified 57 potential subjects with the highest change scores, rank ordered from greatest to least change per MPAI-4. Beginning with the top performers, these individuals were invited to participate in Phase 2. Ten persons consented and interviews proceeded until saturation of themes was confirmed. Interviews were transcribed, coded, and analyzed.
RESULTS
Phase 1
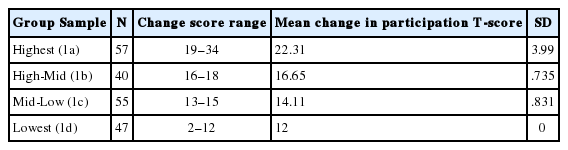
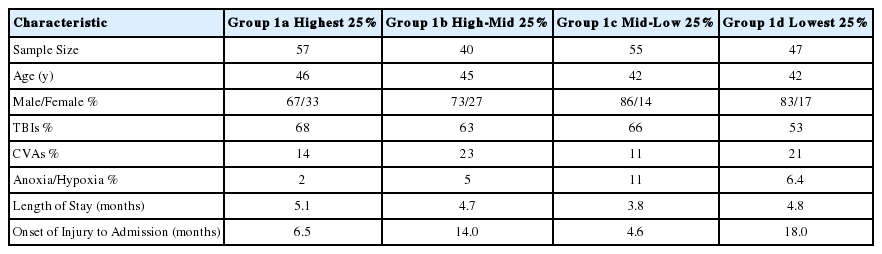
The total MPAI-4 change scores were arranged into four groups: highest (Group 1a); high-mid (Group 1b); mid-low (Group 1c) and the lowest (Group 1d) as shown in Table 2. Table 3 displays participant characteristics.
Beyond data on total T-score change, additional analyses were warranted. The 29 items on the MPAI-4 were converted to T-scores within three subscales: Ability Index, Adjustment Index, and Participation Index. A question to inform Phase 2 of the study emerged: “Which of the three subscales accounts for the most change in Group 1a?” Accordingly, paired T-tests were conducted; improvement on each of the MPAI-4 subscale T-scores (Table 4) was statistically significant, with participation accounting for the most change. This subscale includes: Initiation; Social contact; Leisure and recreational activities; Self-care; Independent living and homemaking; Transportation; Employment; and Managing money and finances.
Further analyses were conducted using a stepwise regression. The six significant MPAI-4 predictor variables [23] of inclusive of self-care, initiation, residence, motor speech, mobility, and impaired awareness were used. Results demonstrated three significant predictors: self-care, initiation, and residence, R2=.87, F(3,53)=113.14, p<0.0001 (adjusted R2=.86). Self-care predicted the largest portion of variance in discharge participation T-score (adjusted R2=.72).
Phase 2
Ten of 57 individuals consented to participate in phase 2. Data were collected via face-to-face, semi-structured interviews. Eighteen process notes were written by the researcher, helping to standardize participant contact, review of informed consent, interview process, and recording. Member checking was completed with two participants, eliciting a 96% agreement that was determined via NVIVO-10 analysis of code coverage. One hundred percent agreement on category and theme descriptions was obtained via member checking. Two peers, both psychologists, participated in calibrated peer review. Each reviewed two different coded transcripts; agreements for these reviews were 98% and 96%, respectively. Once analyzed, data were organized into four categories, each describing a major finding (Table 5).
DISCUSSION
Quantitative findings showed statistically significant improvement in all three MPAI-4 subtest categories, with Participation having the greatest explanatory power. Regression analysis revealed three significant predictors: self-care, initiation, and residence. The self-care finding mirrors the primary focus of rehabilitation programs. Initiation findings suggest that success may be tied to ability to self-initiate activity [23]. Residence (e.g., independent living responsibilities) also maps to areas cultivated in the rehabilitation process.
Qualitative findings illuminated 13 themes within four categories, which represent facets that participants associate with successful outcomes. The themes that contributed to improvement are: paid staff; peers in the program; families of the participants; a higher power; the skills of the paid staff; the ability to assess oneself; particular equipment or techniques; the timing of accessing the PHIDBIR-R program; accessing level of care as part of a continuum; providing different levels of care; following a daily schedule; the physical plant or set up of the program; and location of the program. The results suggest a framework for PHIDBIR-R programming of compulsory construct inclusion, training, supports, and services.
This study confirms that qualitative interviews contribute to a more comprehensive, nuanced insight into survivors’ functional improvement. This research offers important considerations for optimizing functional improvement following brain injury. Illuminated are evidenced-based themes for not only PHIDBIR-R providers, but to stakeholders wishing to improve or establish high quality programs. Undoubtedly, PHIDBIR-R providers should consider these constructs, as themes were identified by the highest achievers as contributors to success. Individuals served, their families and funders, should receive education about these programmatic essentials just as advocates, public policy makers, and the rehabilitation industry might apply these findings to promote optimal outcomes.
Study limitations
Study limitations may include generalizability of results across differing rehabilitation providers or settings.
CONCLUSIONS
The purpose of this study was to reach beyond the traditions of demonstrating an intervention as effective in reducing impairment or disability during neurological rehabilitation recovery. Specifically, identifying the factors that most influence how improvement happens was the focus. The findings of self-care and initiation as the top two predictors of positive outcomes replicated the findings of earlier research [23] and suggest that application of skills is necessary. In addition, the results also support interdisciplinary approaches to complex rehabilitation conditions. However, the qualitative analyses revealed four themes to recovery from the person-centered perspective including support; therapeutic interventions; continuum of care approach; and the physical setting where treatment was provided. The combination of quantitative and qualitative approaches likely provides the best assessment of program and person-centered outcomes. This investigation provides a cogent framework for program development, stakeholder program selection, and advocate and legislator considerations.