INTRODUCTION
Outer hair cells (OHCs) of healthy cochlea work in a non-linear compressive manner to the given acoustic signal such that the softer signals (<50 dB) are provided with higher cochlear amplification as compared to the moderate (>50 dB) and louder ones (>80 dB). This mechanism of cochlear amplification also gives rise to the byproduct, otoacoustic emissions (OAEs) [1]. These emissions of pre-neural origin are measured at the level of ear canal and helps in understanding the micromechanics of the cochlea (Norton, 1994) in normal hearing individuals as well as those with hearing impairment [1–4]. Therefore, OAEs have gained wide acceptance both in clinical practice and research in detecting cochlear hearing loss and as a measure to estimate hearing threshold across different clinical population [3–5].
OAEs can be divided into different subtypes [6], among which distortion product otoacoustic emission (DPOAE) has most often been reported in the literature due to its robustness and reliability [7]. DPOAE is characterized with the peaks and dips across frequencies, known as fine structure. These fine structures are generated in response to the cubic distortion (2f1-f2) of OHCs and therefore acts as a metric in quantifying frequency specific functioning status of OHCs [8].
Mostly DPOAE is interpreted in two ways i.e. DPOAE input/output functions or DP-Gram. Out of these, DPOAE I/O functions can be used to extrapolate DPOAE thresholds using scissor paradigm (Kummer et al., 2000). Using the same paradigm, Boege and Janessen [9] estimated DPOAE thresholds and found 2.2 dB mean difference from that of behavioral pure tone thresholds. Moreover, other studies have also reported the significant correlation between DPOAE thresholds and behavioral pure tone thresholds, signifying its importance in difficult to test population for behavioral measures [10,11]. Furthermore, Hatzopoulos et al. [12] compared DPOAE thresholds of normal hearing individuals with that of individuals with hearing impairment and reported significant correlation between DPOAE thresholds and behavioral pure tone thresholds not only in normal hearing but also in individuals with hearing impairment.
DPOAE has been considered as one of the effective clinical measures in approximating hearing thresholds of mild to moderate severity in infants and neonates where traditional behavioral measures of threshold estimation are less reliable [9–12]. Several studies have reported DPOAE measurements to be a reliable procedure to determine the functioning of OHCs across frequencies [6,13–15]. Hence, to make hearing testing more feasible across different clinical population, lately Distortion Product (DP) threshold test has been introduced as a clinical tool by PATH Medical Device. The procedure is based on the scissor paradigm with cubic distortion of 2f1-f2 in 50 dB HL measurement window. Mehta et al., revealed the test to perform quick assessment and provide frequency specific quantitative information on hearing sensitivity in dB HL [16]. In the study, it was attempted to understand the relationship between DP threshold and pure tone threshold in normal hearing adults. It was found that there was significant difference in the threshold between the two methods with mean difference of 4 dB and 3 dB for right and left ears, respectively. Further, with no reports on the degree of reliability of its DP thresholds values, the extent of confidence in the test results could not be estimated [16].
The generation of distortion product responses may get affected with various factors such as calibration of the device [17], environmental noise, processing limitations in identifying the response [18], probe design [19] and physiological changes related to biological rhythms within individual [20]. Further, quantifying these variables in DP threshold may help in the interpretation of the test results. Also, distortion product responses are reported to have large inter-subject variability and therefore, merely the development of norms may have limited usage [19]. Therefore, along with the estimation of normative values, there is need to examine the test-retest reliability of the DP threshold values across frequencies before it could be assessed in clinical population. Hence, the present study aimed at assessing the DP threshold values across frequencies and examine the test-retest reliability in normal hearing individuals.
METHODS
Participants
Purposive sampling was done in the present study. Fifty normal hearing individuals (100 ears), age ranging from 18 to 30 years (χ̄=24, σ=2.1) took part in the study. All the participants had normal hearing sensitivity as examined with pure tone audiometry. Immittance audiometry revealed normal middle ear functioning for all the participants. None of them had any known presence or history of ear related problems. Individuals with history of ototoxicity or excess noise exposure were excluded from the study. None of them had neurological or vestibular related problems. The procedure of the study was pre-informed to all the participants followed by written consent taken from each of them and all the procedures were performed as per institutional ethics committee in accord with Helsinki declaration (1964) and later amendments.
Instrumentation
Heine 3000 mini otoscope was utilized for otoscopic examination followed by GSI-61 audiometer along with supra-aural headphone (TDH-39) for estimating air conduction pure tone thresholds. Also, bone conduction pure tone thresholds were estimated using Radio ear B-71 bone vibrator. Middle ear status was examined with Path Sentiero immittance meter using the transducer EP-TY 9301769. DP threshold test module which is developed and patented by Path Medical Solutions was employed to measure the DP threshold.
Procedure
All test procedures were done in an acoustically treated double room setup as stated by ANSI-S3.1 (1991) (Frank, 1997). Otoscopic examination was performed wherein only those with intact tympanic membrane and no impact ear wax were considered for the study. Pure-tone audiometry was performed at octave frequencies between 250 Hz to 8,000 Hz for air conduction and 250 Hz to 4,000 Hz for bone conduction using Hughson Westlake Method [21]. Immittance Audiometry was performed to check for any conductive component. Therefore, individuals with ‘A’ type tympanogram and presence of acoustic reflex were included.
DP threshold test was carried out using cubic distortion of 2f1-f2 with constant f2/f1 ratio of 1.2 across 1 kHz, 1.5 kHz, 2 kHz, 3 kHz, 4 kHz, 5 kHz, 6 kHz, and 8 KHz. Further, DPOAE I/O functions was achieved in DPOAE pressure (Pdp). Therefore, the dB SPL level at which Pdp is achieved as zero pascal, is considered as the DP threshold. The DP threshold test assess the functioning of OHCs in 50 dB HL measurement. During these recordings, participants were instructed to sit comfortably in an upright position with minimum movement as possible. The re-assessment of DP threshold test was performed for all the participants after 15 days of the first test in order to understand the short-term reliability [22,23].
Data analysis
IBM SPSS software (version 23) was utilised in the study. The obtained DP threshold data in the present study were checked for normal distribution using Shapiro–Wilk test and so were found to have a non-normal distribution. Therefore, non-parametric Wilcoxon Signed Ranks test was used to assess the test-retest reliability of DP threshold between the two sessions.
RESULTS
All 50 participants tested were found to have normal pure tone average in air conduction thresholds (χ̄=9 dB HL, σ=3.0) and bone conduction thresholds (χ̄=4 dB HL, σ=2.0) across octave test frequencies from 500 Hz to 4,000 kHz. In immittance evaluation, all test ears were found to have tympanometric peak pressure (χ̄=36 mmH2O, σ=23.1) and compliance (χ̄=0.6 mL, σ=0.3) within normal limits.
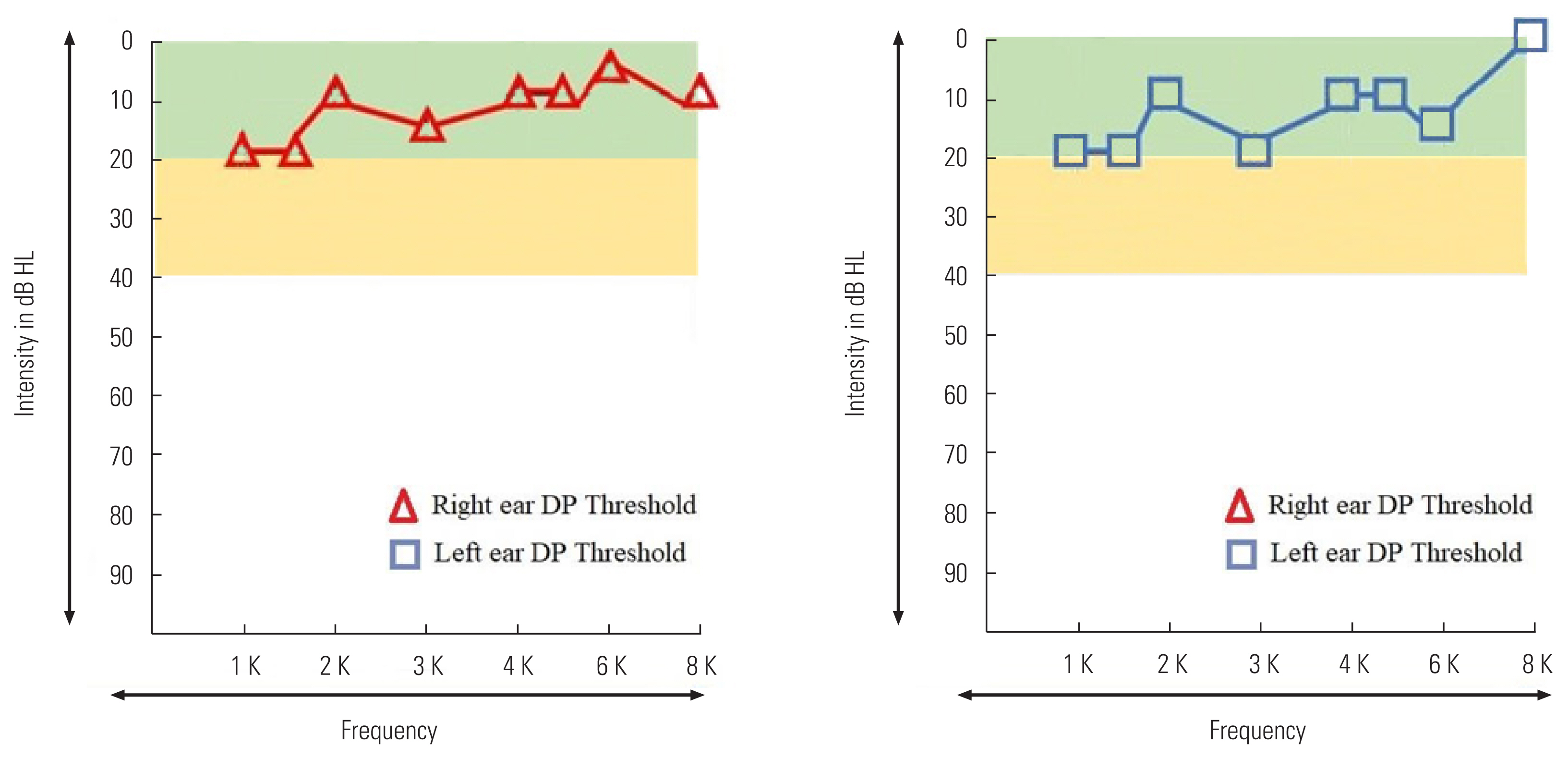
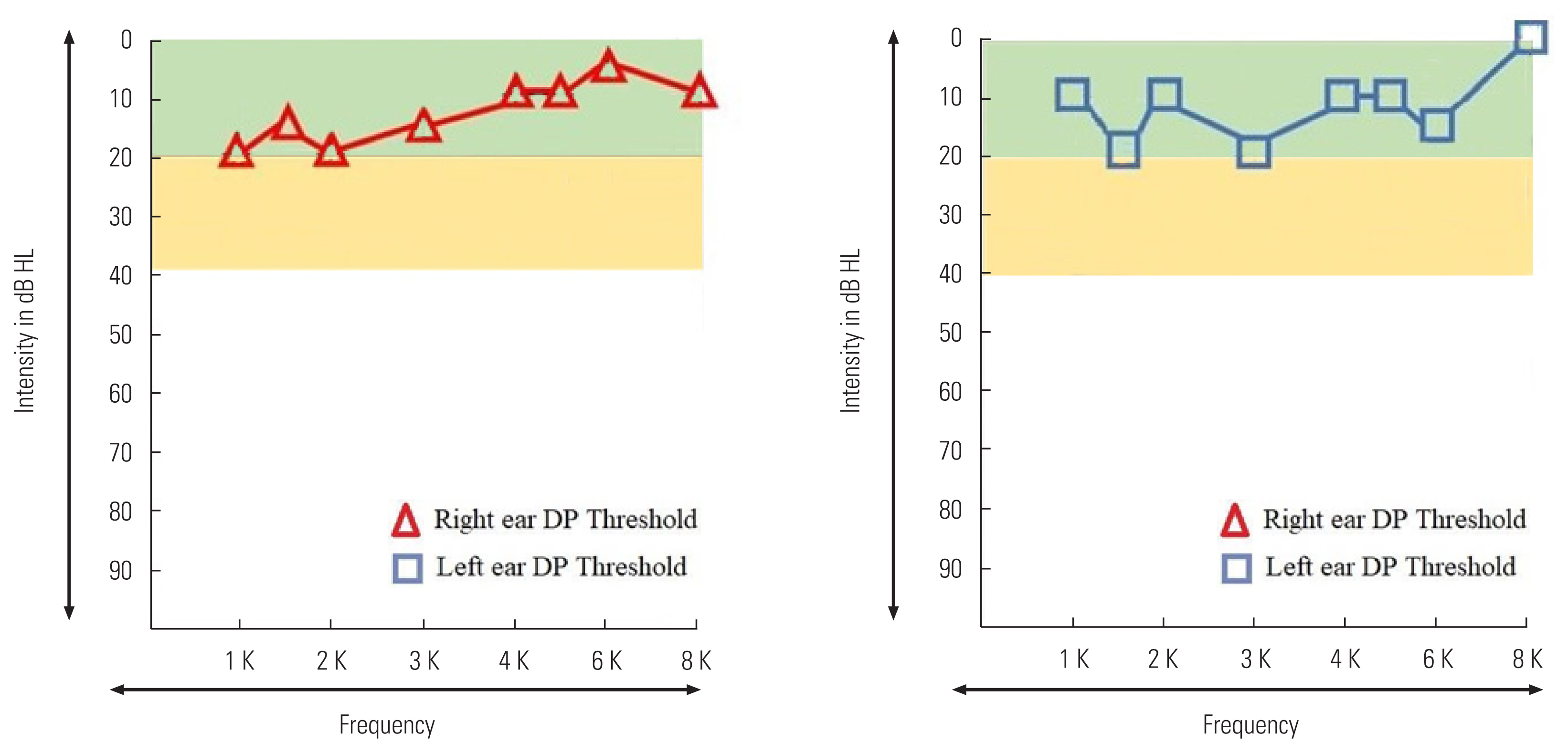
The DP threshold across test frequencies were acquired from all fifty participants in two sessions. The DP thresholds response recorded from one of the participants for the first and second sessions has been illustrated in Figures 1 and 2.
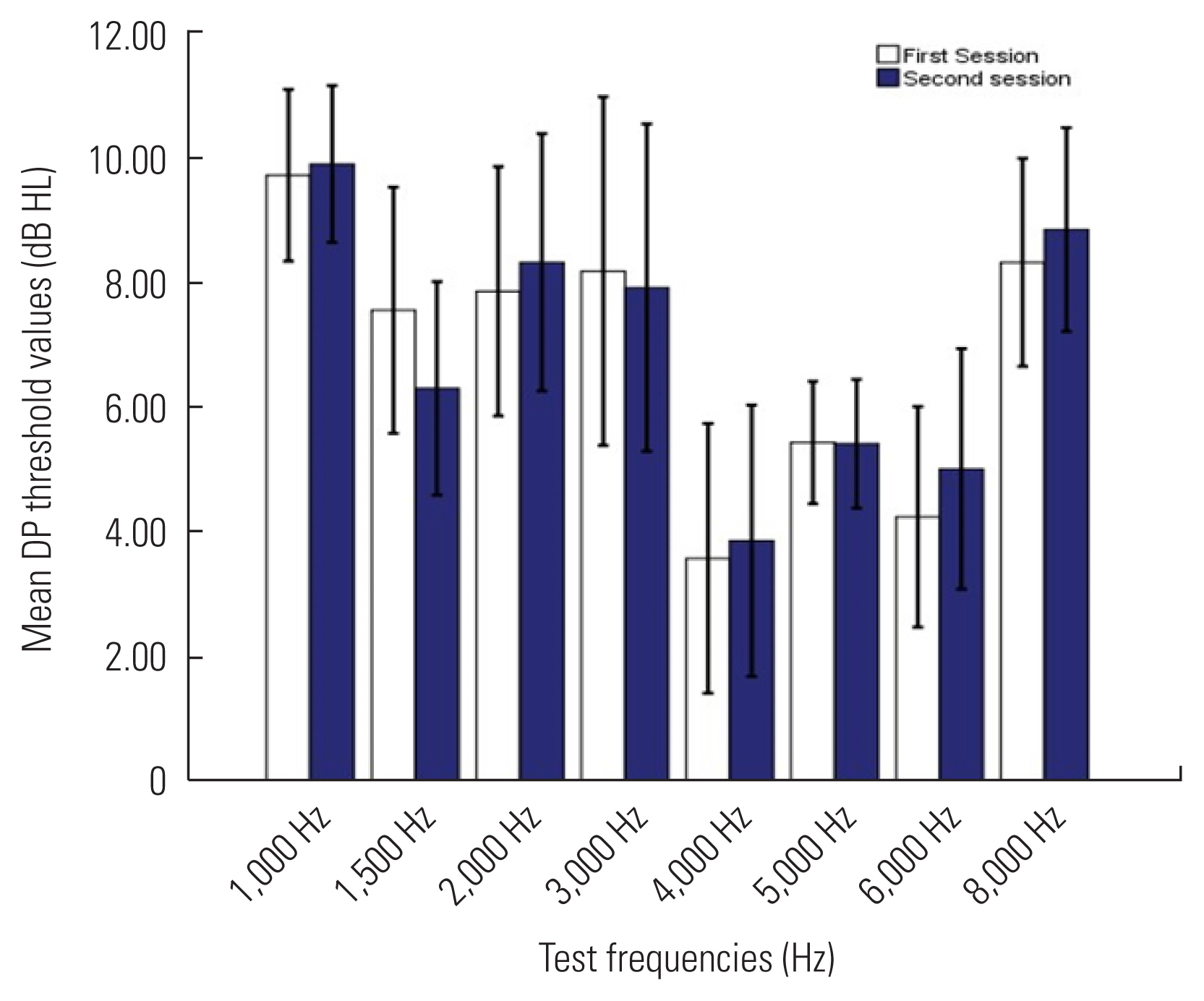
The range of DP threshold level was −5 to 20 dB HL in right ear and −5 to 25 dB HL in left ear across the test frequencies. Descriptive statistics of the threshold values for both ears across test frequencies in two sessions of testing are given in Figures 3 and 4.
In Figures 3 and 4, the mean and standard deviation of DP thresholds across frequencies from 1 kHz to 8 kHz in both ears for sessions I and II are given. The mean DP threshold values range from 2.8 to 9.7 dB HL for right ear (Figure 3) and 2.2 to 9.9 dB HL for left ear (Figure 4) across test frequencies with lowest recorded at 4,000 Hz with higher standard deviation. Moreover, the mean difference across test frequencies between the two sessions were found to range from −0.02 to 1.06 dB HL.
This was followed by Wilcoxon Signed Ranks test which assessed the test-retest reliability of DP threshold between the two sessions as given in Table 1.
In Table 1, it can be observed that no significant difference between the two sessions could be achieved across test frequencies for both ears (p>0.05).
DISCUSSION
The present study examined DP threshold data performed on normal hearing adults in the age range of 18 to 30 years. This is the preliminary study done to establish the normative of DP threshold and the test-retest reliability in normal hearing individuals. Though the hearing sensitivity was within the normal limits, wide range of DP thresholds i.e., −5 to 20 dB HL in right ear and −5 to 25 dB HL in left ear was observed across the test frequencies. Further, it was found to have mean DP threshold ranging from 2.8 to 9.7 dB HL for right ear and 2.2 to 9.9 dB HL for left ear across test frequencies ranging 1 kHz to 8 kHz as given in Figures 3 and 4. These ranges of mean values are comparable with the DPOAE results from earlier studies [24,25]. Wide range of DP thresholds with large standard error can be observed across frequencies responses for both ears in the present study. These variabilities across frequencies can be due to the subject, stimulus, and environment related factors. Environmental and subject related noises are reported to have effect on distortion product responses especially in lower frequency regions. Similarly, the variance in the DP response of mid-frequency region is often attributed to probe refitting, resulting in change in the outer ear resonance to the given stimuli [15]. The current study also revealed relatively lower mean DP threshold value at 4,000 Hz than those measured at other test frequencies for both ears. Also, large standard deviation does persist across higher frequencies in both ears. This can be suggestive of the difficulties in achieving reliable response at higher frequencies. Additionally, the presence of standing wave interference in the ear canal may affect these threshold values [19]. Moreover, the higher frequencies transmission and reception may get affected due to the ear canal acoustics as well as the orientation of probe in ear canal. Therefore, it is often suggested the monitoring of the ear canal volume prior to the fitting of probe, in order to avoid the influence of ear canal resonance [25].
The present study exhibited no significant difference between the two sessions of assessment across frequencies indicating good test-retest reliability of the test. This was suggestive of clinical potency of the tool in monitoring OHCs functioning in various clinical population. Similar result was reported by Franklin et al., where high reliability of DPOAE response was observed between 1,000 Hz and 8,000 Hz for four consecutive weeks and days in normal hearing adults [13]. Moreover, similar findings of invariant test-retest responses were reported in earlier studies as well [15,22,25]. In the present study, though insignificant, there were minor variations in DP thresholds across test frequencies between the two sessions. These could be due to the difference in the placement of probe between the test procedures [15]. This can be avoided to some degree with the usage of calibration marks on probe tips to keep the probe fit constant [22]. Variation in subject related noise between the test sessions may have adverse effect on the DP thresholds to some extent. Though tympanometric status was within normal limits, regular variation in the tympanometric peak pressure among subjects between the sessions could have often given rise to various extent of DP responses [26]. Further, DP responses are reported to get affected by the time of the day when the response was taken [6]. This was not controlled in the present study.
Hence, the current study presents the normative of DP threshold test along with variance, beyond which the fluctuations in OHC functioning can be expected to have occurred. Moreover, it was a preliminary study assessing the test-retest reliability of DP threshold wherein, the retest procedure was performed 15 days after the first test. The results indicated good test retest reliability between the two sessions suggesting immense potentiality of the test in assessing OHCs functioning and can be helpful in differential diagnosis of clinical population including difficult to test population. However, further studies will be of interest to understand the sensitivity of DP threshold test in examining OHCs functioning across gender as well as various clinical population.