Clinical Profiling of Stuttering Characteristics in a Speech Clinic of a Tertiary care Hospital- a Retrospective Study of the Decennial Trend
Article information
Abstract
Purpose
Stuttering is a speech disorder, which affects the smooth flow of speech with a worldwide prevalence rate of about 1%. Reports on the estimation of stuttering prevalence across all age groups based on various influential factors are limited. Clinical profiling of stuttering characteristics in a speech clinic of a tertiary care hospital using retrospective data of 10 years.
Methods
The decennial trend of stuttering between January 2010 and December 2019 with a complete enumeration of stuttering cases across all ages reported in the tertiary care clinic were analysed retrospectively for various factors such as primary and secondary features, and associated deficits.
Results
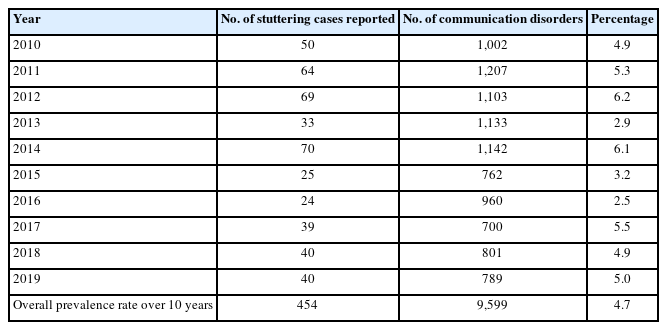
Overall prevalence rate over a 10-year period was estimated to be 4.7%. Descriptive data on characteristics and influential factors related to the occurrence of stuttering were profiled.
Conclusions
This study can be used to understand the decadal trends in stuttering traits. Information about contributing factors can help take steps to prevent risk factors for stuttering. The findings of this study will allow SLPs to understand the need for better documentation and intervention strategies for this population.
INTRODUCTION
Stuttering is a speech disorder, which affects the smooth flow and timing patterns of speech across all ages [1]. In other words, a person who knows what he wants to speak but takes an abnormally long time or abnormal effort to say it [2]. Some of the primary features of stuttering are abnormally high frequency as well as abnormally long duration of the sound, syllable, or word repetitions, an abnormally high frequency, and abnormally long duration of sound prolongations and pauses. A greater percentage of stutterers is first diagnosed between the ages of 3 and 5 years. Stuttering is a condition that affects every ethnic group and exists in every culture [3].
The overall prevalence rate in the developed world is about 1% [4,5]. Epidemiological status of stuttering in the South Wale’s (Australia) community across the life span has reported that around 1.4% of the stuttered population was among the 2–5 years old age group and 1.44% among 6–10 years old with the least noted in the 11–20 age group with a rate of 0.53%. Hence, the overall rate of prevalence was about 0.72%, with a higher predominance rate among younger age groups (1.4%) with the male-to-female proportions ranging from 2.3:1 across all ages [6]. 2.8% of younger children below 5 years, 2.1% among the adult population (21–50 years), and around 3.4% of older children between 6 to 10 years of age are at anticipated risk for stuttering [6]. Stuttering was reported to be more common in males than females [5,6]. A national survey conducted by National Sample Survey Organisation, India [7] reported that around 0.4% of the urban population was prone to stuttering. Within the psychiatric disorders, a prevalence rate of 1.5% was reported between the ages of 4 to 16 years in Bangalore, India and 0.46% with a male-to-female ratio of 4:1 in Tamil Nadu, India [8,9].
Various causal factors have been studied in relation to stuttering, including genetic predisposition, developmental delays, neurogenic causes, and psychogenic factors like stress, embarrassment, and anxiety [10]. The National Institute on Deafness and Other Communication Disorders (NIDCD) identifies a range of variables associated with stuttering, including age, hereditary factors, gender, age of onset, stressors, associated comorbidities, persistency, recovery, and subtypes [11].
The characteristics of stuttering are diverse and encompass a wide range of disfluencies, often accompanied by secondary features related to physical tension or specific speech patterns. Additionally, related behaviors like eye flickers, facial spasms, or breath-holding may be observed [12]. To distinguish between stuttering and typically fluent speech, speech professionals analyze the frequency, duration, and physical tension of speech disfluencies [13]. Characteristics of stuttering include silent, or audible prolongations, repetitions in the expression, blocks which are not promptly controllable; are associated with secondary features related or irrelevant to body structures, or stereotyped expressions and demonstrate different characteristics based on different conditions [10,11]. It is ideal to depict stuttering by quantifying; that is, persistent stuttering is recognized when; disfluent characteristics have continued for more than 6 months; involuntary disfluencies are present; more than 3% out of 100 syllables are disfluent; repetitions in sound, syllable & word level; occurrence of broken words; sound prolongations longer than one second; the presence of block; addition of pitch or volume; related body movements [12]. Stuttering is described as stuttering like dysfluency and other dysfluency. Stuttering like dysfluency is described as a disfluency that involves single-syllable and part-word repetitions, prolongations, and blocks and other dysfluencies include revisions, interjections, and phrase repetitions [13]. There are variations in the stuttering characteristics depending on the number of disfluencies, presence of stuttering-like disfluencies, and the presence of several repetitions [14]. Duration & frequency of repetitions and physical tension are considered as strong distinguishing characteristics of stuttering [15]. People who stutter also exhibit secondary behaviours like “eye flickers, the tension of articulators, tremors of the lips or face, head movements, breathing developments, or clench hand” [16].
In the field of research on stuttering, influential factors have been a topic of extensive exploration. Examination of speech disfluencies in preschool children with and without stuttering aged 3–4 years who were native American English speakers, reported a significant overall difference in total disfluencies (p<0.001) and stuttering-like disfluencies (p<0.001) between the two groups. Additionally, they found a positive correlation between chronological age and time since the onset of stuttering [16]. Another study, investigated factors predicting the onset of stuttering in Australian children, identifying significant associations with family history, birth history, and gender [17]. Study done on stuttering-like disfluencies in Dutch-speaking children, shedding light on frequency, duration, and physical tension as strong differentiating factors [18]. A study done on bilingual German-English speaking children with stuttering revealed variations in the frequency of stuttering between second languge (L2) and first language (L1) languages. It was found to be more in L2 compared to L1. However, Stuttering occurred significantly more frequently on content words compared to function words in L1. No change between stuttering on function and content words in L2. The findings suggest that variations could be attributed to language proficiency. Another study investigated the natural history of stuttering in Australian children up to age 4, identifying factors such as maternal education, sex, and twinning influencing the likelihood of stuttering onset and recovery [19].
Likewise, different factors have been associated with stuttering such as gender, and age, handedness, which can also co-occur with other concomitant factors like speech and language delay, speech sound disorder, specific learning disabilities, intellectual disabilities and even psychosocial aspects including depression, anxiety, poor self-esteem, and emotional instability [21–23]. Onset of stuttering was 8.5% by around 3 years of age with around 51.8% of the various factors including family history, birth history, gender, twin birth status, and environmental factors associated with stuttering onset [24].
Despite the valuable insights contributed by these studies, a notable gap exists in the literature concerning the prevalence trends and influential factors associated with stuttering outcomes in the Indian population. To address this knowledge deficit, the present study aims to conduct an in-depth analysis of retrospective case file records and clinician-client interviews data from a premier healthcare institution in India. By investigating influential factors specific to the Indian context, this research endeavours to provide a comprehensive understanding of stuttering in this population and facilitate evidence-based clinical practice. The hospital where this study was conducted is a premier healthcare center with 2032 beds & serving as one of the largest healthcare facilities in India Its extensive patient base encompasses individuals from the states of Karnataka, Kerala, Goa, Tamil Nadu, Andhra Pradesh, and Maharashtra covering a significant portion of the Southern regions of India (comprising around 19% of India’s area). The Department of Speech and Hearing in this hospital comprises 22 qualified (SLPs) as faculty members, alongside 200 student clinicians. Data for this study is drawn from retrospective case file records gathered during initial assessment interviews with Speech Language Pathologists (SLPs) and their clients. Information pertaining to influential factors is reported through clinician-client interviews, complemented by formal assessments with the Stuttering Severity Instrument [25]. Thus, the data analyzed in this study is anticipated to provide valuable insights and rationale based on a robust sample of cases within this unique Indian context. It is postulated that the decennial trend from this tertiary care hospital can provide a stronger proportion of the overall diseased population reported to the tertiary care centre. Hence, the objective of this study was to estimate the decennial trend in clinical profiling of stuttering in a speech clinic of a tertiary care hospital with a complete enumeration of stuttering characteristics, features, and factors influencing stuttering.
METHODS
Ethical approval
Prior to the initiation of the data collection, approval was obtained from the Department of Speech and Hearing, the Medical Record Department (MRD, No. 67.20), the Institutional Research Committee (IRC), and the Institutional Ethics Committee (IEC: 460/2020). The study was registered under the Clinical trial registry-India (CTRI/2020/12/029789).
Study design
This research utilized a retrospective case review design to analyze data from patient case files at the speech clinic of a premier healthcare institution. Approval was obtained from the MRD of the hospital prior to initiating data collection.
Procedure and data collection
The total number of cases with communication disorders recorded in the speech clinic from January 2010 to December 2019 was 9,599. Among these, 454 cases were identified and diagnosed as stuttering. The data for the study were retrieved from these 454 files. Out of 454 files, 288 files were disposed off from the MRD based on the policy of the hospital, discarding case files not followed up at the hospital after 3 years of the first entry. Additionally, 11 files were excluded due to a lack of information on the assessment reports related to stuttering. A total of 166 files with complete information remained and were considered for further analysis. Hence, for the complete enumeration for profiling the stuttering characteristics were only done from the available 166 files.
The clients’ case files (n=166) were thoroughly reviewed, and relevant data were extracted. The data sources included clinician-client interviews conducted during the patient’s initial visit for assessment. During these interviews, participants provided information on age, gender, geographical location, age of stuttering onset, family history of stuttering, situational variability of stuttering, negative feelings associated with stuttering, and awareness of their speech disfluency. The severity of stuttering and information related to core and secondary behaviors were determined using the Stuttering Severity Instrument-3 (SSI-3) [24]. This information’s were recorded in the files were extracted.
The data recorded in the files were extracted and noted in excel sheets in terms of demographic variables (age, gender, and education level), geographical location, age of onset of stuttering, family history, situational variability, core & secondary behaviours and other influential factors. The data was further analysed for understanding the epidemiological details on age, gender, and education on stuttering populations by profiling the characteristics and associated deficits seen in persons with stuttering. The complete enumeration for profiling the stuttering characteristics were only done from available 166 files.
Data analysis
A total of 454 files were retrieved from the MRD to calculate the hospital prevalence of the stuttering. Further, the collected data from the 166 patients case files were reviewed and analyzed to profile the characteristics of individuals with stuttering and identify influential factors associated with stuttering. This research methodology allowed for a systematic and detailed examination of patient case files, ensuring a comprehensive understanding of the characteristics and influential factors related to stuttering among the study participants.
Statistical analysis
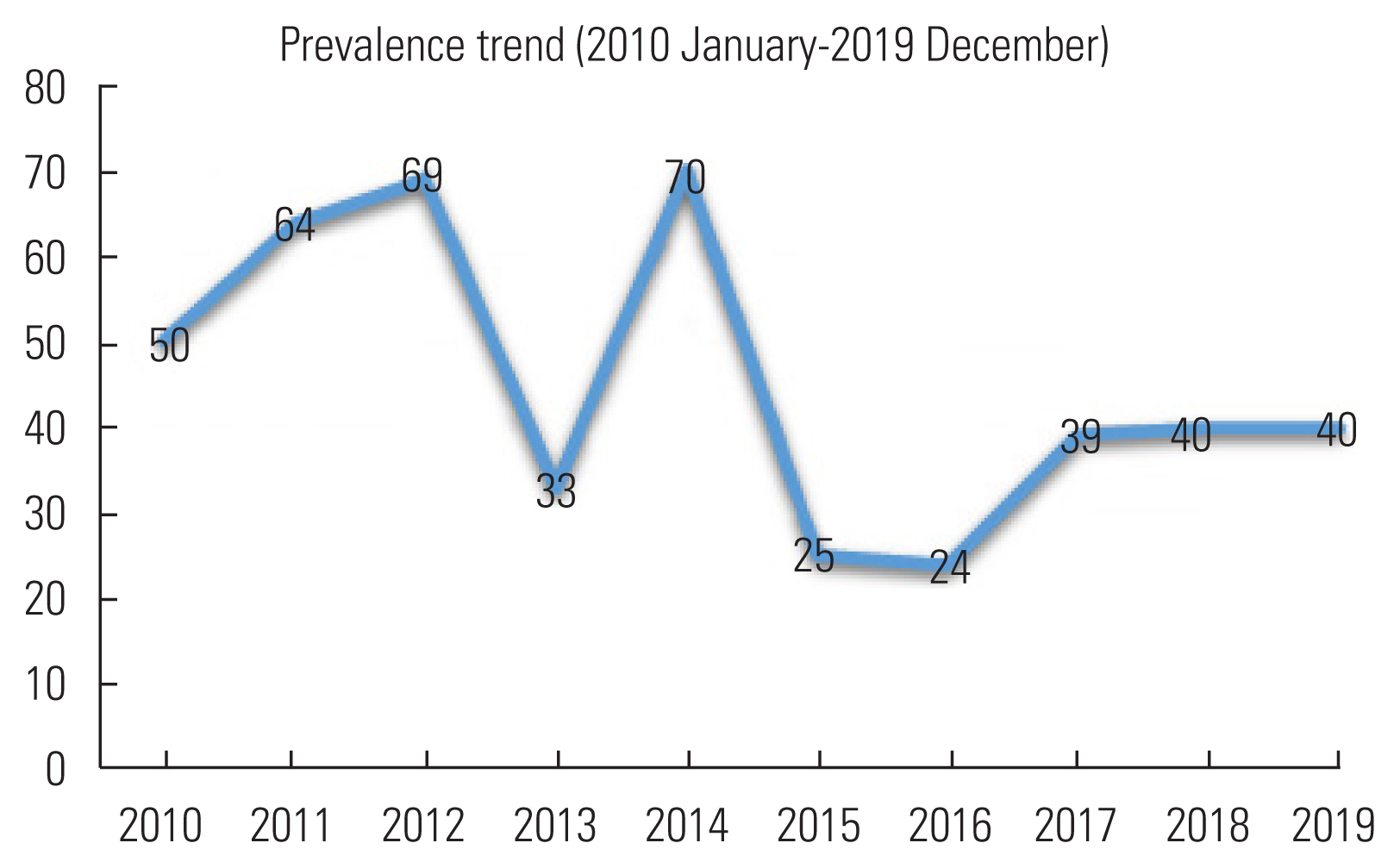
The collected data was organized in an excel spreadsheet. The proportion of stuttering cases reported among all the communication disorders in 10 years was calculated and plotted on a point line graph. The overall period prevalence rate from the available 454 diagnosed case files of stuttering was estimated using the formula: Prevalence rate is equal to the total number of stuttering cases reported in ten years divided by the total number of communication disorders reported to the hospital in ten years multiplied by 100.
Out of the initial 454 files, only 166 files contained completed assessment reports, which were used for profiling the characteristic features of the stuttering group. The data from these 166 files were analysed using descriptive statistics, employing SPSS version 16 software.
RESULTS
The primary aim of this study was to estimate the decennial prevalence trend among the stuttering population in the speech clinic of a tertiary care hospital. Among a total of 9,599 reported communication disorder cases, 454 files were diagnosed as stuttering. The overall period of hospital prevalence for stuttering cases reported in 10 years among communication disorders was 4.7%. During the period (10 years), the greatest increase in stuttering cases was noted in the year 2014 with a prevalence rate of 6.2%. The data also showed that after 2014, there was a decline in the number of cases reported to the clinic, resulting in a prevalence rate of around 3.2%. From 2017 to 2019, the prevalence remained relatively stable, ranging between 4% to 5% (Table 1 and Figure 1).
The secondary aim of this study was to profile detailed characteristics and influential factors related to stuttering from 166 archival case file records retrieved from the MRD.
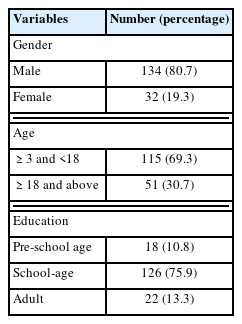
Out of the 166 files reviewed, gender information reflected an overall male-to-female sex ratio of 4.2:1 indicating a higher prevalence of stuttering in males. Regardless of gender, most of the cases (69.3%) were below 18 years (paediatric population). Also, there was a high proportion of the male population (80.7%) as compared to the female. By analysing the data on education, it was found that 75.9% of the population was school-age children (Table 2).
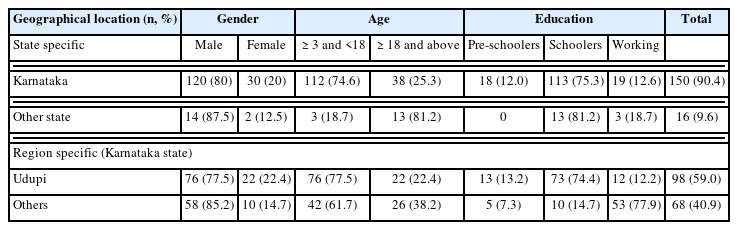
Regarding the geographical location from where most of the cases (90.4%) reported at the clinic were from Karnataka state, with approximately 59% of them originating from and around the Udupi district, as depicted in Table 3.
In majority of the cases (58.4%), stuttering-like disfluencies had their onset in childhood with 90.4% reporting a gradual onset. More than 60% of the cases had positive family history of stuttering and were aware of their stuttering conditions as indicated in Table 4. Analysis of core behaviour showed that repetition was the most common behaviour (94%), followed by blocks (53%) followed by prolongation (36.7%). Among the various secondary behaviours, majority reported movement of extremities as the one common (50.6%) followed by eye blinking (47%). Facial grimaces were the least common behaviours (9.6%) as outlined in Table 5.
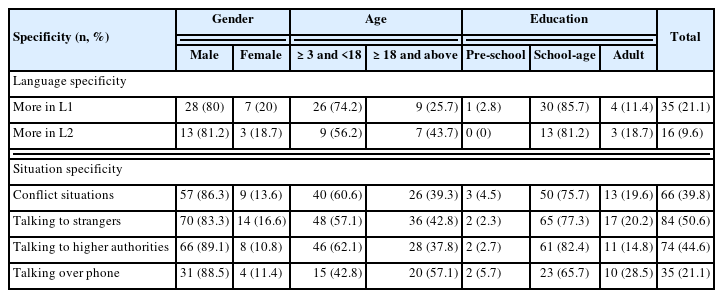
Of the total participant files reviewed, 28.9% were bilingual individuals. Among them, 21.1% reported noticing stuttering-like disfluencies more L1 frequently in their first language, while 9.6% experienced it more in their L2 second language. Notably, stuttering behaviors were more pronounced when speaking to strangers (50.6%) compared to other variations of situation specificity among stuttering population as highlighted in Table 6.
Of the total participant files reviewed 28.9% of the bilingual individuals. Among them, 21.1% of them reported noticing stuttering-like disfluencies more frequently in their L1 language while 9.6% experienced it more in their L2 second language. Notably, stuttering behaviors were more pronounced when speaking to strangers (50.6%) compared to other variations of situation specificity among the stuttering population as highlighted in Table 6.
DISCUSSION
This study estimated the prevalence rate of stuttering among other communication disorders over a 10-year period in a tertiary care hospital. Additionally, the study provided descriptive information on influential factors, characteristics, and variations among the stuttering population. The data was collected retrospectively including both paediatric and adult populations, diagnosed as stuttering at a tertiary hospital located in Udupi district of Karnataka state, India.
The present study revealed that among the total communication disorders cases observed over the 10-year study period, the overall prevalence rate of stuttering cases was 4.7%. This estimation was higher compared to other studies conducted in Australia, USA, and UK, where stuttering prevalence ranged from 0.7% to 1.1% annually [26–28]. The higher difference in prevalence rates observed in this study compared to other reported studies is attributed to the consideration of the overall prevalence rate over 10 years, whereas other studies focused on yearly rates. Additionally, the location of the tertiary hospital, attracting a diverse population from several southern states of India, might have contributed to the higher prevalence observed in this study. The cases reported in the present study included the states of Karnataka (90.4%), Tamil Nadu (2%), Kerala (6%), and Maharashtra (1.6%), covering most of the southern states of India. Other studies conducted in the Indian context are few & one of them has estimated stuttering cases among school children in the Indian population (Tamil Nadu) as 0.46% [9]. Other studies conducted in the Indian context reported stuttering prevalence ranging from 0.4% to 1.5% within specific age groups and geographical locations [7–9].
Regarding gender distribution, the study found that a higher number of stuttering cases were observed in males compared to females, with a sex ratio of 4.2:1. This finding aligned with a previous study conducted in Tamil Nadu, which reported a similar sex ratio of 4:1 [9]. The increment in the male-to-female proportion with age is basic in understanding the recovery and persistent nature of stuttering [29]. Among the participants reported in the present study, 69.3% of cases were below 18 years of age representing the paediatric population. This is similar to the findings that reported 2.1% of the occurrence of stuttering among adults (21–50 years) population [26]. In terms of education, in the current study, it was interesting to note that among the preschool children, school children, and working population, a greater number of cases was seen among school-age children (75.9%). This relates well with other studies [30,31]. This could be attributed to day–to–day demands in school, peer group pressure, teacher identification of disfluencies, and increased parent concerns.
Analysis of influential factors related to stuttering indicated that 58.4% of cases reported that stuttering-like disfluencies emerged since childhood with gradual onset of stuttering. Due to the presence of these disfluencies, persons with stuttering often exhibit adverse feelings and attitudes including negative beliefs about their abilities in speaking [32]. In the current study, 16.3% of the cases reported having negative feelings and attitudes toward their stuttering behaviours including fear, shyness, embarrassment, and shame. There are case reports of increased anxiety levels [33–35]. However, in this study, this could not be documented as no specific anxiety scales to assess the relationship between stuttering and anxiety level were employed. The presence of these negative feelings and attitudes toward stuttering behaviours can affect the person’s overall Quality of Life and highlight the psychosocial nature of stuttering [36,37]. This warrants the need of facilitating appropriate counselling and psychological support for more efficient treatment outcomes. This could be attributed to day–to–day demands in school, peer group pressure, teacher identification of disfluencies, and increased parent concerns.
In the present study, factors like positive family history, fast rate of speech, awareness, and other associated medical conditions were analyzed. It was found that 34.3% reported a positive family history which again emphasized the hereditary nature of stuttering [38]. while very few (3%) reported the presence of associated medical conditions including stuttering associated with traumatic brain injury and stroke. This finding is in concordance with earlier literature reporting that stuttering can occur because of traumatic brain injury and stroke [39,40]. The present study also revealed that 6% reported inadequate speech and language skills due to the presence of articulation and phonological disorders, learning disabilities, attention deficit disorders, and a delay in speech and language development. This is similar to the findings reported that stuttering can co-occur with speech-language disorders and other non-speech-language disorders [41]. Hence, SLPs must be aware of the co-occurring conditions associated with stuttering and their expected effect on assessment and treatment.
Concerning core behaviours of stuttering, the presence of repetitions, prolongations, and blocks were the main distinct core dysfluency characteristics exhibited by stuttering individuals as reported in earlier literature [42,43]. In the present study, all the participants reported the presence of either repetitions, prolongation, blocks, or a combination of these disfluency characteristics. Out of these, 94% of cases reported the presence of repetition as the primary stuttering-like disfluency characteristic. The different types of repetitions depicted by persons with stuttering included sound repetition, syllable repetition, part-word repetition, multi-syllable word repetition, and phrase repetition [13,14,18,44]. In the present study, among the types of repetitions, 90% reported sound repetition, a finding in agreement with earlier reports [45]. There were a few cases in the present study in which, in addition to the core behaviours, dysfluencies such as revisions, incomplete phrases, fillers, and pauses were also observed that were characterized as “hesitant” speech characteristics resulting from the person’s attempt to avoid exhibiting the core behaviours [46]. To obviate the occurrence of the disfluent moment, persons with stuttering exhibit certain struggles, and body movements during a speech which are generally termed as ‘secondary behaviours’ [47]. The secondary behaviours include abnormal breathing patterns, body movements, tremors, and eye blinking [48]. In the present study, among the secondary behaviours noted, 33.7% exhibited head movements, 9.6%, facial grimaces including lip licking, tongue protrusion, lack of eye contact, and nose flaring; 50.6% reported movement of extremities, especially the upper and lower limb movements; 47% of them with eye blinking, and around 22.3%, the tension of articulators. These findings agree with the literature reports [13,15]. It is these characteristics of stuttering like disfluencies with the presence of both core and secondary behaviours which indeed help in differently diagnosing and finding the severity of the stuttering behaviours.
In the present study, regarding language specificity among bilingual participants, 21.1% reported having more disfluency in their L1 language than in L2. This contrasts with the findings reported [49]. where significantly more dysfluency was noted in the L2 compared to the L1 among German-English speakers. The authors recommended that the stuttering pattern presented in L2 was due to the insight of a less proficient (immature) language framework. These variations of disfluency patterns in L1 and L2 in each study may be a result of several other factors like language complexity, language dominance, and language familiarity [50].
Data from this study has indicated that multiple factors may influence the onset and persistence of developmental stuttering, emphasizing the multidimensional nature of the disorder [51]. Therefore, the findings from the present study highlight the clinical profile of stuttering over ten years and its complexity. The current study further needs to be explored prospectively to understand the numerous elements considered as risk factors influencing the outcome of the disorder and planning up appropriate intervention strategies.
Limitation
The retrospective phase of the study includes the enlistment of participants from Karnataka, Kerala, Goa, Tamil Nadu, Andhra Pradesh, and Maharashtra which only covers most of the southern regions of India. A few case files were disposed of due to the discarding procedures in the MRD of the hospital. Hence, only a moderate sample of 166 files was incorporated for detailed investigations compromising the statistical effect. In addition, information related to anxiety levels, the overall impact on quality of living, and speech naturalness were not documented in the case files. Notwithstanding these constraints, this is the principal study to date on stuttering which assessed the prevalence across ten years performed in India and is the first to profile these numerous characteristics and factors related to stuttering. However, the treatment strategies used and follow up information’s were not analyzed as they were not documented in the case files.
CONCLUSION
Each country needs a tenable measure for the prevalence of stuttering to outline its public arrangement and viably address the effective management of the issue. The overall estimated cases of stuttering over the last 10-year period (4.7%) and the decennial trend individually in each year in the present study demonstrate increased awareness of this disorder across each year. The findings of this study would enable SLPs working with this population in understanding the requirements for better documentation & intervention strategies for this population. Since this study included a population of all ages, along with the paediatric population, it is equally important that young adults with stuttering should also be provided with speech services to rid them of their problem. This study also provided information on various factors influencing stuttering including family history, age of onset, awareness, rate of speech, presence of associated conditions, language specificity, secondary behaviours, and core behaviours which determine the importance of analyzing these factors during assessment as well as for implementing effective treatment strategies for person with stuttering. Consequently, the information from the current study reveals the expanding event of stuttering as well as various domains that should be considered while clinically dealing with this specific population. Accordingly, this information could be considered for developing an assessment protocol for stuttering as futuristic endeavours.
Clinical implications
The findings of the current study can be utilized to understand the decennial prevalence trend and various domains associated with stuttering. The information on influential factors may help in receiving measures to forestall risk factors of stuttering. Likewise, these findings can be considered in the preparation of a standard protocol for stuttering assessment that can be inferred for effective intervention strategies.