Enhancing swallowing quality of life in older individuals after the oropharyngeal strengthening exercise
Article information
Abstract
Purpose
Older individuals may be vulnerable to swallowing disorders due to age-related neuromuscular changes. Although older individuals have swallowing difficulties, they can improve swallowing by the preventive exercise of swallowing. The purpose of this investigation was to examine whether the oropharyngeal strengthening exercise (OSE) has effects on swallowing quality of life in older individuals.
Methods
Twenty-seven older individuals performed a 4-week OSE using a home-based and self-administered procedure. They completed the Swallowing Quality of Life questionnaire (SWAL-QOL) before and after a 4-week OSE program. Statistical comparisons were made using a matched pairs t-test (p<0.05).
Results
The total scores of the swallowing quality of life questionnaire significantly improved after a 4-week OSE. In addition, participants perceived that physical symptoms related to swallowing were significantly improved after a 4-week OSE. Particularly, frequency of choking during eating was significantly reduced after a 4-week OSE.
Conclusions
The OSE contributes swallowing quality of life in older individuals. It may also benefit patients with dysphagia in terms of patient perspectives.
INTRODUCTION
Changes in swallowing occur in all adults over time. Physical changes in older individuals are associated with increased risk for disordered swallowing [1–6]. It is estimated that 40% of adults aged 60 and older currently suffer from swallowing difficulties [4–6]. This high percentage is associated with the motor and sensory functions of swallowing that change with age and age-related disease. Healthy older adults do not present swallowing disorders, but neurologic and neuromuscular age-related changes may increase the risk for swallowing disorder. This phenomenon is referred to as presbyphagia [7]. Presbyphagia involves neuromuscular degeneration of anatomy, physiology, sensory feedback, motor control, and central processing of swallowing [8–11].
Although they can compensate and adjust their swallowing performances based on their necessities, changes in swallowing function influence their quality of life [12,13]. Older individuals are sociable and desire to have opportunities to share mealtimes during social occasions [14,15]. Changes in swallowing make the older individuals hesitate socializing during mealtime given the safety, health, and social issues that arise with swallowing dysfunction, thereby decreasing the quality of life in this population. It is important to sort out which characteristics are related to aging in order to develop appropriate diagnostic and treatment strategies for this population. In addition, the changes in swallowing function may provide insights in understanding onset and progression of disease in this population.
Current swallowing intervention focuses on rehabilitation in patients with dysphagia using compensatory and rehabilitation strategies. Studies that evaluate the effectiveness of a preventative approach for those with a high risk for swallowing disorders are lacking. The risk of swallowing disorders is increased for older individuals. This investigation hypothesized that a preventative swallowing intervention will have a positive effect, because a strengthening exercise for swallowing muscles would increase muscular and swallowing reserve in older individuals. This investigation evaluates the value of a preventative approach by developing an oropharyngeal strengthening exercise (OSE) applied using home-based and self-administered procedures. The OSE combined two swallowing exercises: tongue strengthening exercise and effortful swallow. Both tongue strengthening exercise and effortful swallow have been reported to have positive effects in the older population and/or patients with dysphagia [16–20]. Tongue strengthening exercises are performed by pushing the tongue against the hard palate in patients with weakness of the tongue. Robbins et al. [20] conducted a tongue strengthening exercise in stroke patients for 8 weeks. They reported the tongue exercise even had effects on the quality of life related to swallowing from the patients’ perspective. For subcategories of the swallowing quality of life questionnaire, fatigue, communication, and mental status were improved after the tongue strengthening exercise [20]. Effortful swallows can be applied to facilitate the pharyngeal stage of swallowing. According to Hind et al. [18], effortful swallow increases the duration of laryngeal vestibule closure, protecting the airway for a longer time and decreasing the risk of aspiration. Previous investigations focus on effectiveness of one target treatment maneuver on muscle activity and strength rather than the quality of life related to swallowing [19,21]. More research is needed to identify the effectiveness of an intervention program on the overall quality of life.
The purpose of this study is to identify swallowing quality of life using the Swallowing Quality of Life questionnaire (SWAL-QOL) [22] after a 4-week OSE program using a home-based and self-administered procedure in healthy older individuals. The SWAL-QOL helps the investigator to understand the functional status of activities related to swallowing in healthy older individuals. This investigation is expected to have dual effects of the OSE from both the tongue strengthening exercise and the effortful swallow.
METHODS
Participants
Twenty-seven healthy older participants were included. The participants consisted of 23 females and 4 males. The mean age of participants was 73 years old and the age range was from 58 to 85 years. Participants met from the following inclusionary criteria: a) above 55 years old, b) normal oral structure and function, c) no history of swallowing impairment, d) no history of neurologic or head and neck impairments, and e) nonsmokers or discontinued smokers for at least 5 years. Participants were excluded if they reported a) oral sensory deficits and b) undergoing treatment or taking medication that affects their swallowing function. Informed consent was given by all participants prior to study initiation.
Study design and interventions
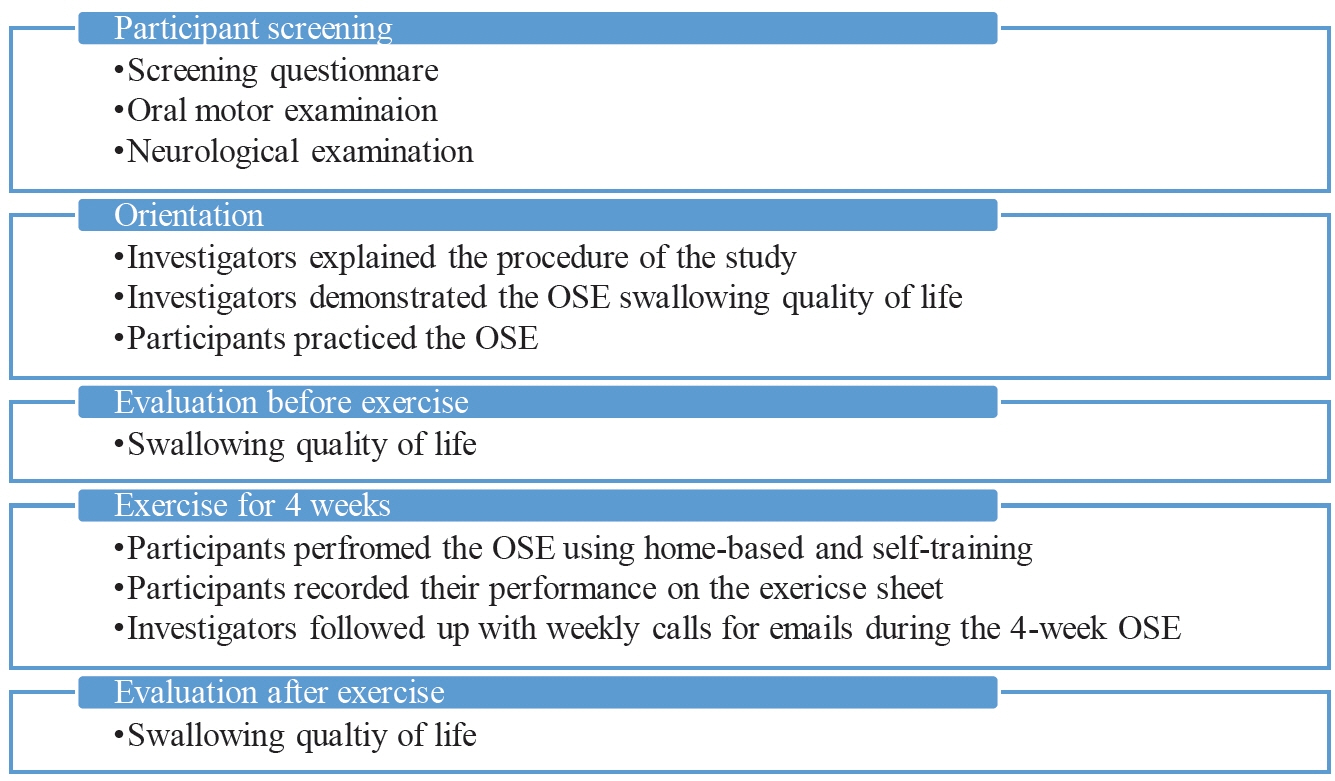
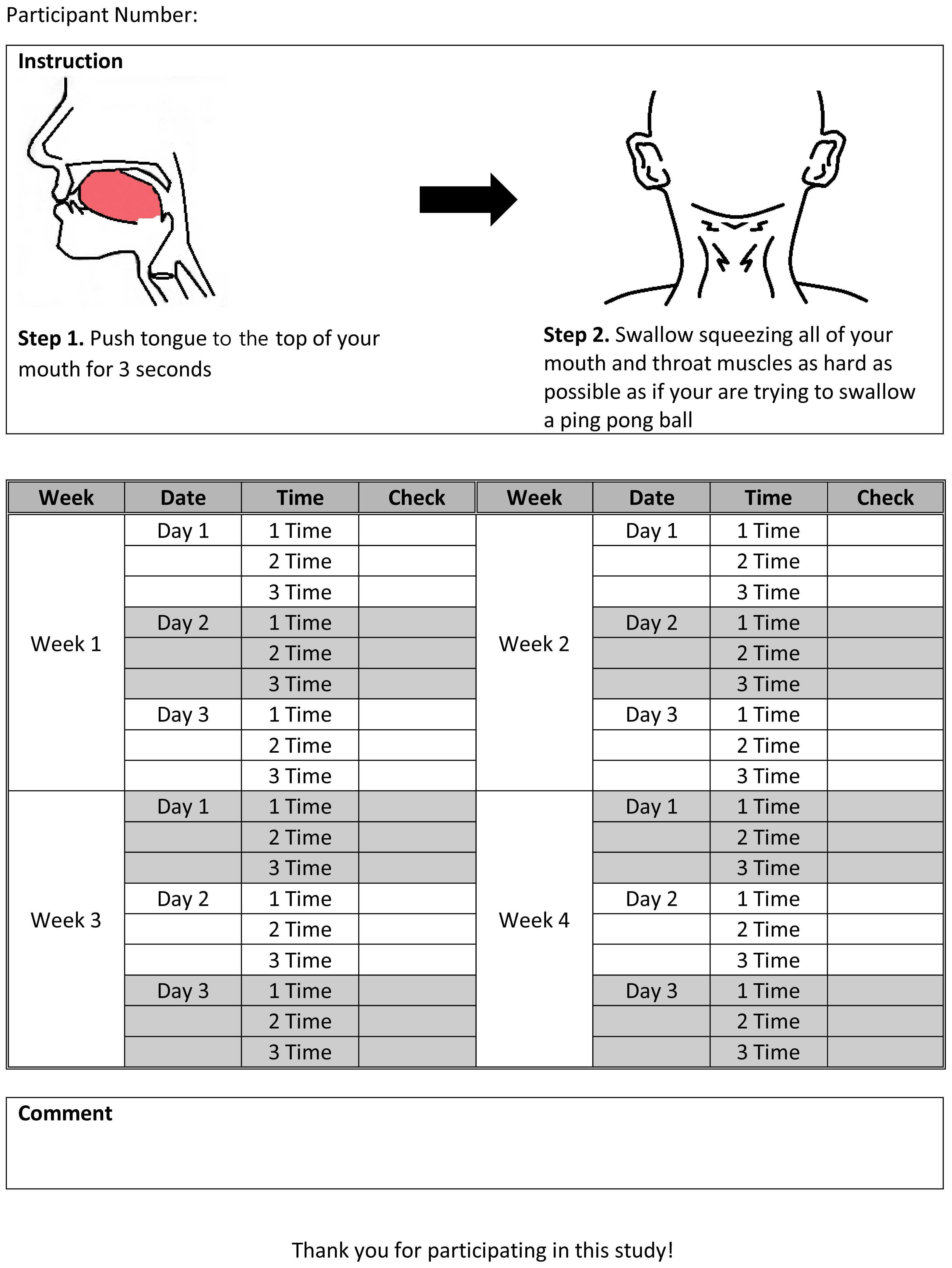
The study protocol was approved by the institutional review board of Ohio University. The intervention was conducted by speech-language pathologists. Investigators pre-screened participants for eligibility through the questionnaire, oral motor and neurological examinations were also completed prior to an orientation. The participants who met the inclusion criteria had two in-person sessions and 4-week of home training sessions. Two in-person sessions consisted of an orientation, data collection at baseline and after the OSE. In the first in-person session, the investigators demonstrated the OSE and the participants practiced the OSE at least 10 times with investigators. The OSE was a combination of a tongue strengthening exercise and an effortful swallow exercise [24]. The instruction of the OSE was “Put your tongue behind your upper teeth, and feel that ridge there? That is where your tongue normally goes when you take a swallow. The tongue pushes the food or liquid back into your throat. Put your tongue behind your upper teeth or top of your mouth and push hard for 3 seconds, and then swallow. As you swallow, I want you to squeeze all your mouth and throat muscles as hard as possible as if you are trying to swallow a ping pong ball or a boiled egg.” Participants performed OSE 10 times per session, 3 sessions a day, on 3 days per week for 4 weeks using the home-based and self-administered training program. During 4 weeks of OSE, participants recorded their date and completion of performance on the exercise sheet (see Appendix A) and the investigator and her assistants contacted each participant by email or phone call every week. The participants completed data collection session after 4-week of the OSE. Figure 1 presents the flowchart of the investigation procedure.
Outcome measures
The SWAL-QOL questionnaire provided information regarding the effectiveness of the exercise and was applied to compare the quality of life from the patient’s perspective with physiologic function. SWAL-QOL included a total of 44 items and 11 subcategories (fatigue, sleep, burden, eating desire, eating duration, symptoms frequency, communication, fear, mental health, social functioning, and food selection). SWAL-QOL used the Likert method of scaling. Each item was given a score from 1 to 5 [23].
Each participant’s SWAL-QOL [22] scores were collected before and after the exercises. Each participant was allowed ample time to fill out the SWAL-QOL and pose any questions they might have. The investigator assisted in completing the SWAL-QOL for participants who did not understand questions in the SWAL-QOL. The swallowing quality of life questionnaires were measured before and after the OSE program using the same procedures. The investigator was blinded to participant identity and condition at all times, and examined and analyzed the SWAL-QOL.
Data analysis
Total scores and percent of subcategories’ scores in SWAL-QOL were submitted for analysis. Total scores were calculated by sum of scores for each item. Subcategories’ scores were calculated to percent by using the below formula to control equally comparable values, because each subcategory included different number of items.
Statistical analysis
The SWAL-QOL questionnaire provided continuous data. Pre-and post-exercise scores of all SWAL-QOL data were compared using a matched pairs t-test to measure the intervention effects (p<0.05).
RESULTS
The total scores of the swallowing quality of life questionnaire were significantly different for the baseline and after a 4-week OSE (t(26)=−3.129, p=0.004). The mean of total scores at baseline was 199.04 and standard deviation was 16.08. The mean of total scores after a 4-week OSE was 200.81 and standard deviation was 15.41.
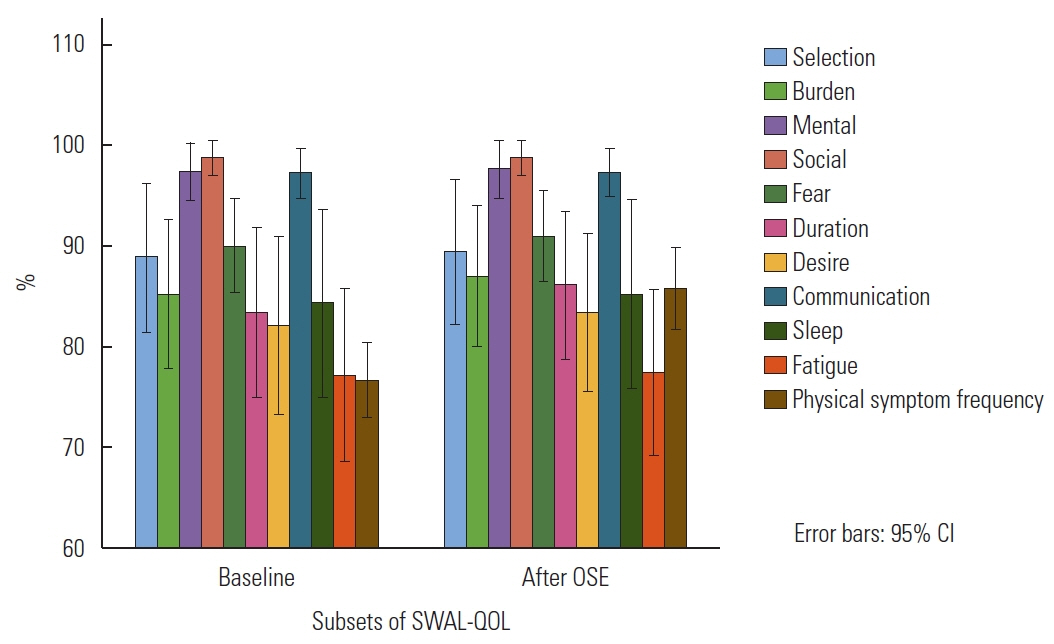
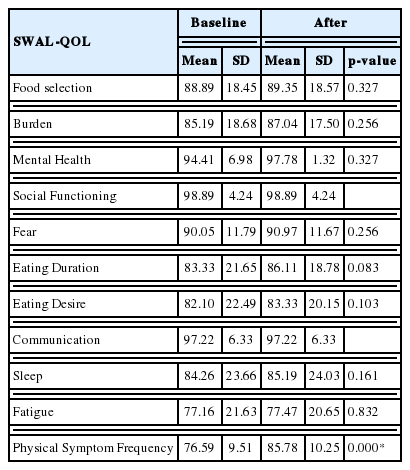
In subsections of SWAL-QOL, the means of percentage in eating duration, desire, sleep, and fatigue after a 4-week OSE were greater than baseline. Means of percentage of food selection, burden, social functioning, and communication were not different between baseline and after a 4-week OSE. The percentage of each subcategory is presented by Figure 2. Table 1 provides the mean and standard deviation of all percentage scores for each subsection.
There was no significant difference in all subcategories of SWAL-QOL except in the frequency of physical symptoms associated with swallowing difficulties. The frequency of physical symptoms associated with swallowing difficulties was significantly reduced after a 4-week OSE (t(26)=−13.414, p<0.01). In the frequency of physical symptoms associated with swallowing difficulties, the number of participants who answered “often choking during eating” was reduced from 4 to 1 after a 4-week OSE. Also, the number of participants who answered “never choking during eating” was increased from 9 to 11 after a 4-week OSE. Frequency of choking during eating food was significantly reduced (t(26)=−2.302, p=0.03). Frequency of participants choking during eating is presented by Figure 3.
DISCUSSION
The purpose of this study was to examine swallowing quality of life (SWAL-QOL) after a 4-week oropharyngeal strengthening exercise (OSE) using home-based and self-administered procedures in healthy older individuals. Qualitative effects of a 4-week OSE program were identified by using the SWAL-QOL questionnaire. According to results of the SWAL-QOL responses before and after a 4-week OSE, the 4-week OSE program influenced overall swallowing quality of life, physical symptoms associated with swallowing difficulties, and frequency of cough during eating.
Among symptoms associated with swallowing difficulties, frequency of coughing during eating was significantly reduced after training with the OSE for 4 weeks. This result suggests that the OSE program has a positive influence on airway protection. Robbins and colleagues in 2007 reported the effect of the tongue strengthening exercise for 8 weeks on SWAL-QOL and airway protection using the Penetration-Aspiration Scale (PA scale) in stroke patients [20]. Stroke patients after the 8-week tongue strengthening exercise demonstrated decreased PA scale scores, which indicated reduced airway invasion of liquid as well as reported reduced frequency of coughing on liquid. This result of the investigation suggests that the OSE may improve airway protection of food or liquid in older individuals.
The data of SWAL-QOL may provide insight to pre-symptomatic signs and impact of signs made by the OSE in terms of overall health and dysphagia associated with swallowing quality of life for older individuals. The results of subsections in SWAL-QOL presented relatively lower percentages of scores in burden, eating duration and desire, sleep, and fatigue. Among these subsections, eating duration and desire are in need of being carefully observed in older individuals. Eating duration and desire vary between normal and degenerative diseases, such as Parkinson’s disease; and this variation can vary as a result of the severity of degeneration. All subsections except sleep were significantly different between healthy older individuals and individuals with Parkinson’s disease; furthermore, eating duration and desire were reduced when comparing early stage Parkinson’s disease and later stage Parkinson’s disease as well as younger and older individuals [25]. The present study supports the suggestion by Leow and colleagues in 2010 that SWAL-QOL can provide information on influence of healthy aging and alert health care professionals for future problems by observation of pre-symptomatic signs [25].
In addition, previous researchers who assessed swallowing quality of life using the SWAL-QOL questionnaire reported different physical symptoms associated with swallowing difficulties among several subsections. Leow and colleagues [25] reported that older individuals showed more physical symptoms associated with swallowing difficulties than younger individuals. There was a similarity in the findings of Leow and colleagues and this investigation. Percentage score for symptom frequency in older individuals was 91% while for this investigation was 86% after the OSE program [25]. Questions on symptoms of swallowing difficulty were similar for symptoms such as choking, saliva, chewing difficulty, and food sticking in the oropharynx. This finding provides additional support that the older participants experienced more physical symptoms associated with swallowing, such as choking, saliva, chewing difficulty, and food sticking in the oropharynx than the younger population.
The ultimate goal of the OSE is to improve swallowing function and quality of life in older individuals who are vulnerable to swallowing disorders and patients who suffer from swallowing disorders. The findings in this investigation showed promising potential in using a preventative approach for older individuals. Earlier direct intervention such as the OSE might have an effect on swallowing. Additionally, the OSE can be efficiently executed in terms of time because the OSE was home-based and utilized self-administered training. Participants were able to manage their training time, and the OSE did not require participants to commute to a clinic. This investigation supports feasibility of home-based intervention. This investigation has several limitations such as its small sample size and that it was only a 4-week program. Additional studies with larger participants are warranted to identify the effects of swallowing quality of life. In addition, future research would be to identify effect on swallowing quality of life after swallowing exercises for substantial periods in patients with dysphagia due to stroke, Parkinson’s disease, and head and neck cancer.
CONCLUSIONS
According to the participants’ perspectives, the 4 weeks of the OSE program had positive effects on swallowing quality of life. For effects of the OSE in swallowing quality of life, participants reported reduced frequency of physical symptoms associated with swallowing difficulties. Particularly, frequency of choking during eating was reduced. The results of SWAL-QOL provided qualitative data on effects of health-related quality of life, although the participants’ responses of SWAL-QOL were unable to fully provide the independent effect of swallowing through the OSE. The qualitative data using the SWAL-QOL questionnaire addressed the impact of the OSE beyond objective measures. This investigation suggested one of the possibilities to assess swallowing in terms of individuals’ perspectives with intervention. Especially, for those with a combination of several diagnoses, both objective and subjective assessments support to understand patients with swallowing difficulties from various angles [26]. This investigation will help promote earlier identification and preventative intervention of dysphagia in older individuals who are vulnerable to swallowing disorders. The findings from this investigation suggested the feasibility of home-based and self-administered training for preventative swallowing intervention.