Speech handicap and vocal tract discomfort with different types of face masks in the COVID-19 era
Article information
Abstract
Purpose
Compulsory use of masks is recommended to prevent droplet infection during the COVID-19 pandemic. This can alter optimal communication in daily life. This study compared the self-perceived speech handicap and vocal tract discomfort when wearing and not wearing a face mask and different types of face masks in a healthy population.
Methods
This is a cross-sectional study conducted via an online questionnaire. Speech Handicap Index (SHI) and Vocal Tract Discomfort Scale (VTDS) scores were collected via Google forms (Google, Mountain View, California) from 128 healthy Korean populations with and without face masks and different types of face masks.
Results
While speaking with a face mask, subjects were identified with a significant lack of air, unclear articulation, and reduced speech intelligibility in a noisy situation. Although total SHI and VTDS scores exhibited slightly higher with a face mask, no significant differences were found between with and without mask conditions. For mask type, individuals who frequently wore KF94 masks subjectively perceived significantly higher speech handicap and vocal tract discomfort than surgical or fabric masks.
Conclusions
In the current study, wearing a face mask did not have a significant impact on speech handicap and vocal tract discomfort in a healthy adult population during the COVID-19 pandemic period, implying people already adapted to wearing a face mask. In terms of speech problems and frequency, the severity of sensation or symptoms of vocal discomfort significantly differed depending on which face mask type they used. Future research should address self-evaluation of their feeling or experience due to face mask use, considering the elderly and patients with communication disorders who suffer more with communication in daily life.
INTRODUCTION
During the COVID-19 pandemic, masks have played an essential role in minimizing the spread of diseases and reducing infections, and most countries are currently required to wear face masks in certain situations [1,2]. In each country, various types of masks and respirators are commercially available, including standard masks (e.g., N95, FFP2 masks), surgical mask, and fabric mask. Depending on the effective filtering, the N95 or KF94 mask has the highest barrier level, and the surgical mask has similar protection characteristics to the N95 mask [3]. Current recommendations from the Centers for Disease Control and Prevention (CDC) and WHO include social distancing of at least 6 ft [4] to minimize exposure to the coronavirus and protect one from the risk of infection, completely covering the nose and mouth in public, and wearing a mask to fit the face tightly. Unlike KN95 or KF94, surgical and fabric masks protect against relatively large droplets and do not require a tight seal [5].
Although masks can protect individuals from droplet blocking and viral infections, masks can negatively affect communication in daily life [6]. Several studies demonstrated that face masks interfere with the transmission of speech signals when covering the speaker’s mouth and nose. For instance, higher speech frequencies, such as /s/ and /∫/, are affected by the face mask [5], and the type of mask affects the speech signal [6]. Goldin et al. [7] found that face masks attenuated the sound levels at frequency regions between 2 and 7 kHz by 3–4 dB for the surgical mask and 12 dB for the N95 mask compared with no face mask. Thus, speaking while wearing a face mask decreased the clarity of speech signal, which resulted in degraded speech intelligibility, and consequently increased listening effort, especially in background noise and speech perception [8–10]. Moreover, it is also difficult for the speaker to show facial expressions and accurate non-verbal pragmatic intent for effective communication interaction with the listener [11]. Presumably, the higher the barrier level a mask can provide, the greater its impact on the voice and speech signals.
More than two years after the COVID-19 pandemic, little research has been conducted on the speech difficulty or vocal tract discomfort perceived by individuals who have adapted to wearing masks to some extent in their daily lives. To date, self-evaluation tools are invaluable in investigating the individual’s perspective in evaluating voice and speech disorders [12]. Through self-evaluation tools, therefore, it is possible to know an individual’s perception of the effect on speech problems or quality of life due to the use of masks. Initially, the Speech Handicap Index (SHI) developed by Rinkel et al. for measuring the psychosocial speech impact of oral or pharyngeal cancer in patients is a transformation of the Voice Handicap Index (VHI-30) for adults by Jacobson et al. [13] to match the speech problem [14]. It consists of a total of 30 questions, including the psychosocial (P) function with 14 items, the speech (S) function with 14 items, and others with 2 items, and each item related to speech problems in daily life was measured using a 5-point scale from 0 to 4.
In addition, the vocal tract discomfort scale (VTDS) is a self-evaluating questionnaire for the subjective evaluation of voice disorders, proposed by Mathieson in 1993. It is measured on a numerical scale from 0 to 6 using eight qualitative descriptors in terms of the frequency and intensity of symptoms, including the terms burning, tight, dry, aching, tickling, sore, irritable and lump in the throat [9]. Both questionnaires are validated and used in Korea [10,11].
In terms of self-evaluation perspective, several studies were conducted through the use of some questionnaires they developed or voice handicap index, vocal fatigue index, and vocal tract discomfort scale to detect their self-perceived vocal change [19–22]. Furthermore, most studies analyzed healthcare workers and other groups who use face mask during their working hours [19,20,22].
It was still unknown how much wearing a mask caused speech problems or difficulties in people’s daily lives. Moreover, it is worthy to look at the discomfort of vocal tract or speech difficulties normal people perceive due to the use of masks during the COVID-19 pandemic.
Thus, this study aimed to investigate self-awareness of speech-related handicaps and throat discomfort when wearing and not wearing a face mask, especially concerning wearing different types of face masks in a healthy population.
METHODS
Design and participants
This is a cross-sectional study. A questionnaire was created with Google forms and distributed on social media in Korea. A total of 132 healthy Korean populations responded to the survey—14 males (11%) and 118 females (89%)—and all participants agreed to the consent form for the participation in this study. Among the participants, three males and one female, who reported they had voice problems, were excluded from the subjects.
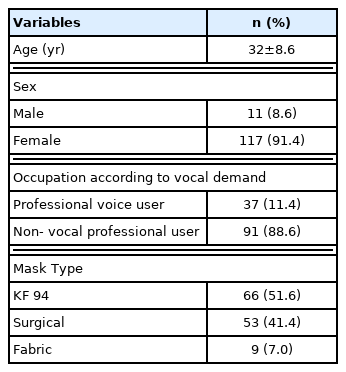
Finally, 128 respondents were eligible to answer the questions, including demographic information (age, sex, profession) and mask type they usually use daily (Table 1). They completed the self-evaluation of their speech problems and vocal tract discomfort with mask and no mask conditions, respectively.
Korean version of the SHI and VTDS
The Korean version of the SHI [15] and the Korean version of the vocal tract discomfort scale [17] were included in the questionnaire in order to measure the self-perceived speech handicap and throat discomfort. The SHI consists of 30 total questions divided in to 2 domains, the speech function and psychosocial function subscale. Among SHI questions, 1, 2, 3, 5, 6, 9, 10, 13, 15, 18, 20, 21, 26, and 28 items are about speech function, and the speech function score was obtained by adding the scores of these questions. In addition, 4, 7, 8, 11, 13, 14, 16, 17, 19, 24, 25, 27, 29, and 30 items related to social psychosocial functions were calculated by adding the scores of these questions. 22 and 23 items were included only in the total score.
For VTDS, all participants evaluated the frequency and the severity of their symptoms/sensations in terms of burning, tight, dry, aching, tickling, sore, irritable, and lump in the throat.
The SHI questions were measured using a 5-point scale (0=never, 1=rarely, 2=sometimes, 3=often, 4=always), and the VTDS used a 7-point scale (0=none, 6=always) for the frequency and severity of sensation and/or symptoms, indicating that the higher the score, the more speech problems there are. All participants rated the speech-related difficulties and throat discomfort they experienced by selecting a value with and without wearing a mask, respectively.
Statistical analysis
The means and standard deviations were calculated using descriptive statistics for the total K-SHI score and subscale scores. Paired t-test was carried out to compare the total K-SHI score and subscale scores with and without wearing a face mask within the same individual.
Pearson correlation analysis was conducted to examine the correlation between the total SHI score and the subscale score (speech and psychosocial) when wearing a mask, respectively.
Furthermore, to compare whether there is a difference in SHI scores depending on the type of face mask, a non-parametric Kruskal-Wallis test was conducted because most of the Kolmogorov-Smirnov results did not satisfy normality. All the statistical analyses were conducted using IBM SPSS Statistics for Windows version 23.0 (IBM Corporation, Armonk, NY). The significance level was .05.
RESULTS
Face mask type
The mask type most frequently worn was KF94 with 66 (51.6%) out of 128, followed by surgical masks with 53 (41.4%) and fabric masks with 9 (7.0%) (Table 1).
Speech problems related to face mask type
The mean SHI scores (total [T], speech [S], and psychosocial [P]) without wearing a face mask were 7.01 (T), 4.39 (S), and 1.98 (P), while with wearing a face mask 7.14 (T), 4.71 (S), and 1.82 (P). However, there were no significant differences in total K-SHI scores (t[127]=−0.271, p=0.787), as well as in all scores of K-SHI subscales, including speech (t[127]=−0.955, p=0.342) and psychosocial (t[127)]=0.831, p=0.408) between with and without wearing a face mask. On the other hand, some items showed significant differences when the K-SHI scores with and without wearing a face mask were compared. Specifically, items 2 (“I run out of air when I speak”), 9 (“My articulation is unclear”), and 10 (“People have difficulty understanding me in a noisy room”) were significantly higher when wearing the face mask (p<0.05) (Table 2).

Results of the paired t- test, comparing each item for the Speech Handicap Index with and without mask conditions in healthy populations
In addition, the total score revealed a significantly high positive relationship with speech function (r=0.964, p=0.000) and social psychological function (r=0.934, p=0.000) with mask-wearing, respectively.
Table 3 also shows the nonparametric Kruskal-Wallis test results for K-SHI total and subscale scores among the different types of masks. The main effect of mask type in total K-SHI scores and subscale scores (speech, psychological) was significant (p<0.05). Post-hoc comparisons revealed that all K-SHI scores were significantly higher in the KF-94 mask compared to the surgical or fabric mask.
Vocal tract discomfort related to face mask type
The frequency of sensation or symptoms of the discomfort of the vocal tract tended to increase to 3.89±5.9 when not wearing a face mask while 4.16±6.6 when wearing a face mask, but there was no statistically significant difference (t[127]=−0.664, p=0.508).
Regarding the severity of symptoms of vocal tract discomfort, the results revealed 3.57±5.50 in the unmasked condition and 3.88±6.26 in the masked condition. The VTDS did not differ significantly between unmasked and masked conditions (t[127]=−0.817, p=0.415).
There was a significant impact of the main effect of mask type on the frequency-total (p=0.004) and severity-total (p= 0.006) of sensation or symptom of vocal tract discomfort (Table 3). Individuals with KF94 masks exhibited significantly higher frequency and severity than surgical and fabric masks (Figure 1). Among the subscales of VTDS-frequency, the effect of mask type significantly differed for tight (p=0.019), dry (p=0.020), tickling (p=0.009), and lump in the throat (p= 0.008). Moreover, for VTDS-severity, there were significant differences in dry (p=0.019), tickling (p=0.009), and irritable (p=0.049) with different types of face masks.
DISCUSSION AND CONCLUSION
The current study aimed to investigate the self-perception of speech difficulties and sensations or symptoms of vocal discomfort caused by using masks in healthy speakers during the COVID-19 pandemic. As a result of this study, there was no significant difference between wearing a mask and no mask situation, which is considered to have been adapted to wearing a mask to some extent, unlike the early stages of COVID-19, as wearing a mask became mandatory due to COVID-19. Although no differences in total SHI score between no mask and mask use condition were exhibited, some items in the K-SHI significantly differed. For example, items 2 (“I run out of air when I speak”), 9 (“My articulation is unclear”), and 10 (“People have difficulty understanding me in a noisy room”) showed significant differences with and without wearing a face mask, which were related to breathing, articulation, and noise situations when speaking. Several studies also revealed that speech intelligibility was significantly impaired with wearing a mask [3].
Furthermore, the high-frequency region plays an essential role in the perception of clear speech [3], and masks can lead to articulatory limitations and restrict the projection of voice or speech sound. It may then be more difficult to articulate clearly when wearing a face mask than when not wearing a mask. Therefore, these SHI items were sensitive items indicating speech problems when wearing a face mask.
In previous research, Nuria and Filipa measured the Voice Handicap Index (VHI), and they found significantly higher voice-related handicap when using a face mask in the VHI total score and scores for all dimensions between two different countries during the COVID-19 compulsory facemask use period from the middle of October 2020 until the middle of January 2021 [16].
The VHI difference was higher for the item “People have difficulty understanding me in a noisy room” (functional dimension) in Portuguese and Spanish speakers. This result demonstrated that item 10 (“People have difficulty understanding me in a noisy room”) of SHI, similar to the VHI question, was significantly higher in this study’s current outcome, which showed the same results as a previous study [16]. In addition, the mask type and total daily use time can also contribute to higher VHI-10 scores [17].
In this study, there were no significant differences in total and subscale scores between with and without wearing a face mask for speech handicap but the type of mask affected the speech handicap. The KF94 mask showed a significantly higher speech-related handicap in the SHI total score and all dimensions (speech and psychological), although there are many types of KF94 masks. This fact shows that people who use masks are believed to have adapted to speech or vocal patterns to some extent, but they still increase their perception of voice or speech changes depending on the type of mask.
Several studies analyzed the self-perception of vocal effort and voice-breathing coordination during wearing face masks, a significant increase in vocal effort perception, communication difficulties with mask condition, especially with the particular case of healthcare workers who mainly reported tiredness, voice impairment, and avoidance of voice use during and after a long work-day [19,20]. Furthermore, healthcare professionals wearing masks reported greater vocal symptoms post-workday compared to pre-workday compared to post-workday [22] and significantly greater amounts of vocal effort in the masked condition [23].
Thus, the total daily time of use and the occupation related to professional voice use may affect voice or speech difficulties depending on whether the mask is worn or not. In this study, non-vocal professional users were more included. From this point of view, it is very valuable to look at the changes in speech or voice that normal population perceive due to the use of masks in their daily lives.
In addition, this study found no significant differences between the conditions of wearing and not wearing a mask while speaking in relation to the frequency and severity of K-VTDS. However, the frequency and severity of sensation or symptoms in vocal tract discomfort people perceived were affected by mask type.
KF 94 mask users were present with tight, dry, tickling, and lump in the throat more frequently and were more severely recognized as dry, tickling, and irritable, implying that individuals who wore KF94 masks felt more frequent vocal discomfort, while those who frequently wore surgical masks experienced less vocal discomfort. Clinically, the terms of “tight” and “lump in the throat” indicate musculoskeletal discomfort, related to muscle tension dysphonia or hyperfunctional dysphonia while “Dry” refers to possible mucosal changes [24]. When speaking with a face mask, both nose and mouth are covered by the face mask protective layers, leading to obstruction of the upper airway. The Ministry of Food and Drug Safety permits a non-drug health mask under the name Korea Filter (KF). KF refers to the classification of the dust collection efficiency, which means the performance of blocking fine particles, that is, the ratio of masks filtering test particles, into 80–99%. Currently, health masks are classified as KF80 if more than 80% of NaCl particles are blocked according to the dust collection efficiency of the filter, KF94 if more than 94% are blocked, and KF99 if more than 99% of NaCl particles are blocked.
The face intake resistance is 60 Pa or less or 6.2 mm H2O or less in the KF80 mask, whereas the KD94 mask is 70 Pa or less or 7.2 mm H2O or less, implying the face resistance of the KF94 mask is greater. The leakage rate of the face area, which is the rate of air leakage through the gap when wearing a mask, is less than 25% for KF80 masks and less than 11% for KF94 masks, while surgical masks have fluid resistance due to waterproof effects and can be worn loosely. According to the Korean Ministry of Food and Drug Safety, surgical masks and droplet blocking masks have the same waterproof effect because they undergo the same liquid resistance experiment, and thus have similar particle blocking capabilities [25].
Due to the spread of COVID-19, the use of KF94 and surgical masks has increased significantly in Korea, and the better the fine dust blocking effect, the harder it is to breathe, especially when speaking with KF94 masks, which is interpreted as inducing more effortful phonation or vocal misuse when speaking and raising awareness of voice and speech changes.
Overall, given these results, SHI total, subscales (speech, psychosocial), VTDS severity and frequency found to have significant differences on the mask type. That means mask type may critically impact the current study’s self-perception in speech and voice-related problems. Further research is required to investigate the effect of masks on speech and voice for various factors (e.g., smoking, occupation, age, patients with speech or voice disorders, etc.) that can affect mask use.