|

|

AbstractPurposeAn unexpected pandemic ‘COVID-19’ has arisen in the world which affected many lives either directly and/or indirectly. Coronavirus disease 2019 (COVID-19) is an acute respiratory illness caused by the newly identified β-coronavirus SARS-CoV-2 virus.
MethodsCOVID-19 has proven challenging to the public health system. Taking into account thehearing healthcare, an internet based survey was conducted to understand the effect COVID-19 has on the usage of hearing aid among its users during the pandemic and conditions such as lockdowns arise due to it. This study was carried out by the Department of Audiology, MAA Institute of Speech and Hearing, India, during the period of June-August 2020. The questionnaire consisted of 13 questions, developed and presented via “Google forms”. The questions in the questionnaire was based on the presumptive but common problems faced by the hearing aid users. The nature of the questions was specifically focused on the effect that pandemic and the resultant lockdowns have on the hearing aid usage. The survey was self-administered and the time taken would be 5–10 minutes. The respondents were asked to answer the survey with the best of their experience.
INTRODUCTIONAn unexpected pandemic ‘COVID-19’ has arisen in the world which affected many lives directly and/or indirectly. Coronavirus disease 2019 (COVID-19) is an acute respiratory illness caused by the newly identified β-coronavirus SARS-CoV-2 virus [1]. At nearly 106 million cases worldwide, the pandemic is declared a global public health emergency [2]. As there was no vaccine or standard treatment for COVID-19, social distancing (including reduced interpersonal and community interaction) may be the only way to minimize disease transmission.
COVID-19 has proven challenging to the public health system. COVID-19 outbreak has impacted mental health leading to stress, anxiety, depression, insomnia and suicide in the worst case [3]. In this frightful scenario additional attention should be given to people with existing other medical conditions/impairments/disabilities, one in such are the individuals with hearing loss. There are 3 major impact of COVID-19 on individuals with hearing loss; they are forced to an extra conditions of isolation (social distancing and quarantine) apart from the one they face from having hearing loss, information and resources regarding COVID-19 are not always easily accessible for hearing impaired people [4] and hearing health care service delivery not radical enough to support COVID-19 condition.
Most services in hearing healthcare especially those provided by Audiologist (hearing aid trial, hearing aid programing, hearing aid repair, hearing aid accessories, hearing training, cochlear implantation, cochlear implant mapping, cochlear implant repair, cochlear implant accessories and auditory verbal therapy) does not come under medical emergency services and therefore were not easily available to the individuals with hearing loss during the pandemic. Fortunately, there were few services (such as, for sudden onset hearing loss, sudden onset of vertigo and sudden device (Cochlear implant/Hearing aid) failure which were incorporated as emergencies where a patient can reach out to Audiologist immediately for assistance [5].
During these unique times of social isolation, communication is essential for one’s mental health and well-being, whether talking with someone over the phone, participating in a video chat, or simply listening to the television. Hearing loss affects 466 million people globally [6] which means that COVID-19 pandemic would have impacted communication of such a large number of people with hearing loss.
Although COVID-19 pandemic had impact on everyone, individuals with hearing loss exhibit considerable problems, particularly when there is limited access to their hearing care providers. Considering hearing healthcare services, the focal point in the present study was on understanding the effect of COVID-19 pandemic on hearing aid users and their communication needs. Therefore, an internet based survey was conducted to know the problems encountered by the hearing aid users.
METHODSThe study was carried out at the Department of Audiology, MAA Institute of Speech and Hearing, India, during the period of April-August 2020. The survey consisted of a self-administered questionnaire (Appendix 1) that included total of 13 questions which were developed and revised over several drafts with inputs from 5 senior Audiologists. The draft was initially piloted on 10 individuals (5 Audiologists and 5 hearing aid users). The individual observation of these respondents and their comments about the questions were used in revising the survey questions and response-choices. After several revisions, a final draft was prepared for web upload and presentation to the hearing aid users. The survey was presented online via ‘Google forms’ and an e-mail link was sent to the existing hearing aid users of our patient database. Respondents were asked to answer the questions to the best of their experience. The questions were YES/NO and multiple choice questions where choice was also permitted to report one or more problems. All the participants were contacted through mobile phone and consent was obtained for participation and publication of data.
The questions included in the survey were based on the common problems faced by the hearing aid users. Nature of the questions was generally focused on how COVID-19 and lockdowns affected hearing aid usage & what measures were adopted to overcome them. Overall survey could be answered in less than 10 minutes. Initial questions included age, number of years of hearing aid usage and whether they were using hearing aids unilaterally or bilaterally. Other questions focused on the issues like hearing aid usage duration, hearing aid maintenance and accessories, hearing aid programming, difficulty wearing hearing aid with mask, whether mask affected communication and sanitization of hearing aids. Finally, the respondents were asked for suggestions on how they would get better treatment in pandemic COVID-19 condition.
RESULTSA total of 147 respondents participated and presented us a complete survey report. The respondents varied considerably in terms of age range which was between 20–80 years (Table 1). Among them, 72.6% were using aids bilaterally and 27.4% unilaterally. Maximum percent of respondents were 41 to 70 years of age. All the survey respondents had significant experience in hearing aid usage (Table 2).
Following the declaration of COVID-19 as pandemic, 72.8% of the respondents thought that they were going to face problems with their hearing aid usage during the pandemic conditions and where as 27.2% thought otherwise (Figure 1). Majority of the respondents had reported that they initially though thought that they are going to face problems like maintenance of hearing aid (67.3%), accessories (69%) and hearing aid programming (45.1%). Below 1% initially thought that they will be problem with online hearing training, fine tuning & trouble-shooting of hearing aids (Figure 2).
During the COVID-19 conditions, the usage of hearing aid was increased for 72.6% of the respondents while 24.4% reported reduced usage of the hearing aids. The respondents who reported increased hearing aid usage (Figure 3) mentioned following reasons for the increased usage; increased communication with family & friends (82.6%), increased television time (70.6%), increased conversation over phone (47.7%) and job related increase (0.9%). Other 24% respond ents who reported decreased usage reasoned less communication requirements at home (71.7%), no social gatherings (61.7%) and not watched television (26.7%) as the cause of decreased usage (Figure 4).
Figure 5 shows the responses towards the various problem (that were put up in the survey) that might have occurred during the COVID-19 condition. Sixty-four percent of the respondents reported that they faced problem with the hearing aid maintenance, where as 36.2% did not. Seventy-two percent of the respondents faced problem with accessories like batteries, ear tips and receivers. Hearing aid programming issues were also reported by 59.6% of the respondents. One more uncommon question (except for pandemic situations, people generally don’t wear mask) was asked about wearing hearing aids along with masks. Sixty-six percent of the respondents found difficulty while using hearing aid with the mask. As a consequence of mask, majority of respondents (63.9%) found difficulty while communicating to others and 27%. About the sanitization of hearing aids, fifty percent of participants responded positively as they did sanitize their aids.
DISCUSSIONAlthough COVID-19 has adverse effects on every human, this particular study was conducted to understand how COVID-19 conditions including lockdowns has affected individuals with hearing loss especially the hearing aid users. Web based survey done in this study revealed that COVID-19 had impacted Audiological services necessary to the hearing aid users. COVID-19 has also affected their communication needs. The focal point observed through the survey was that, the respondents reported COVID-19 significantly affected them in a variety of ways. It is important that they are aware of these consequences and have enough knowledge to communicate to the world.
Overall survey results showed that majority of the respondents faced variety of problems with their hearing aid usage during the COVID-19 pandemic condition. Majority of the respondents faced problems more what they face in usual non-pandemic conditions. They reported lack of access to the Audiological services that has hindered their communication needs. It was suggested by the respondents that guidance on the maintenance must be carried out properly, consistently and constantly by professionals in order to prevent technical failures of devices in a more scientific approach during these kinds of pandemic situation.
One important finding was that masks were causing difficulty in communication. It is well understood that face coverings are an obstacle to effective oral communication. Face masks are also found to act as a low-pass acoustic filter which interferes with speech. Goldin et al. [7] suggested that the sound pressure levels for 2,000 to 7,000 Hz were decreased by 3–4 dB for a common medical mask and up to 12 dB for the N95 mask. The combined effect of decreased intensity, speech perceived as more muffled, environmental noises, and lack of visual cues will certainly cause speech perception problems for many people with hearing loss.
There was one more concern that ‘Stay home and Social distance’ would result in increased loneliness, depression and other related health problems. A recent scientific report stated that 43% of adults aged 60 or older in the United States reported feeling lonely. It is well known that social isolation and loneliness can become more common with age, and this is often due to the onset of hearing loss or cognitive decline [8]. If any individual has people experienced substantial levels of loneliness before the COVID-19 pandemic, it’s well understood that feeling will be more in COVID-19 conditions.
Due to lockdowns with limited Audiological services, patients couldn’t attend important follow-ups for their hearing aid programming, which subsequently affected their hearing aid performance. Hearing aids are typically programmed for each individual patient in an Audiology clinical set-up which was shut down during the COVID-19 lockdowns. During lockdowns, Tele-Audiology (Audiology Telemedicine) came as an alternative to provide hearing services. Tele-Audiology refers to the delivery of hearing related services via telecommunication technologies. Tele-Audiology services included services such as evaluation, assessment, monitoring, prevention, intervention, supervision, education and consultation [9]. The use of telemedicine in hearing healthcare is relatively new and the applications include patient education and diagnostic services [10]. There were multiple studies that have investigated the delivery of Tele-Audiology services in a variety of settings. These studies reported that programming of hearing aids could be performed effectively and efficiently [11]. No serious adverse events were reported. However, degradation of audio and/or video quality in the communication link hindered interactions between providers and patients [12]. Other challenges in the Tele-Audiology services are related to the issues of connectivity, technology/equipment, dedicated staff, costs involved and licensing issues. Irrespective of these challenges Tele-Audiology results in improved patient care, enhance patient satisfaction, extended reach of Audiology services and reduced travel time [13].
To conclude, COVID-19 crisis has directed that hearing health care requires radical rethinking of service delivery in Audiology. This crisis has prompted hearing professionals to think about how telemedicine can be best utilized in the field of Audiology in future. It has also created the momentum to rapidly formulate innovative digital Tele-Audiology approaches (including Web and App-based hearing solutions/tools for remote device troubleshooting, counseling, fine-tuning, and tracking usage) in response to these changing situations.
CONCLUSIONSCOVID-19 has negatively affected the lives of many people with hearing loss in a variety of ways. This study suggested considerable impact of COVID-19 on hearing aid users. We suggest the exploration of more innovative methods to put into Audiology practice to meet the needs of hearing impaired people. In conclusion, further research to provide effective solutions and global strategies needed in these kinds of pandemic conditions.
CONFLICT OF INTERESTCONFLICT OF INTEREST On behalf of all authors, the corresponding author states that there is no conflict of interest. Figure 1Illustrates percentage (%) of respondents who thought they are going to face problems related to hearing aid usage during COVID-19. 
Figure 2Illustrates the respondent’s initial thought on what kind to challenges they would face in terms of hearing aid usage during COVID-19. 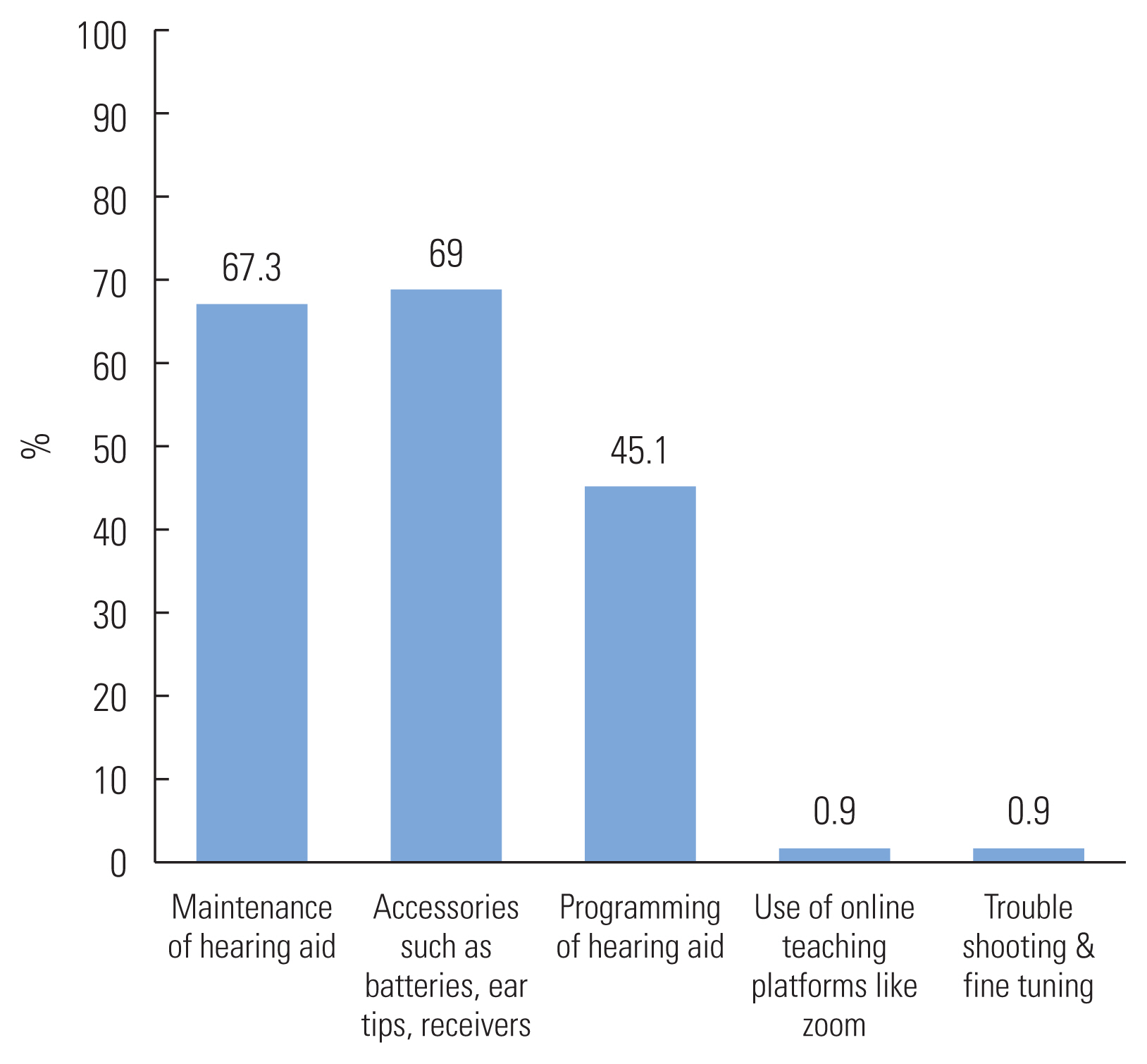
Figure 5Respondents responses towards the various problems that might have occured during the COVID-19 condition. 
REFERENCES1. Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses. 2020;12:372.
3. Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry. 2020;66:317–320.
4. Trecca EM, Gelardi M, Cassano M. COVID-19 and hearing difficulties. American Journal of Otolaryngology. 2020;41:102496.
5. The Audiology Method. 2020.
https://www.theaudiologymethod.com/blog/2020/4/14/navigating-covid-19-withhearing-loss-resource-guide
.
6. World Health Organization. 2020. Deafness and Hearing Loss.
https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss#:~:text=Over%205%25%20of%20the%20world'swill%20have%20disabling%20hearing%20loss
.
7. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? Hearing review. 2020;27:8–9.
8. AARP. 2020. How to Fight the Social Isolation of Coronavirus.
https://www.aarp.org/health/conditions-treatments/info-2020/coronavirus-social-isolation-loneliness.html
.
10. Pearce W, Ching TY, Dillon H. A pilot investigation into the provision of hearing services using tele-audiology to remote areas. Australian and New Zealand Journal of Audiology. 2009;31:96–100.
11. McElveen JT Jr, Blackburn EL, Green JD Jr, McLear PW, Thimsen DJ, Wilson BS. Remote programming of cochlear implants: a telecommunications model. Otology & Neurotology. 2010;31:1035–1040.
12. Goehring JL, Hughes ML, Baudhuin JL, Valente DL, McCrery RW, Diaz GR, et al. The effect of technology and testing environment on speech perception using telehealth with cochlear implant recipients. Journal of Speech Language Hearing Research. 2012;55:1373–1386.
13. Ballachanda B. Telepractice in audiology. Audiology Online. 2019;24859.
|
|
|||||||||||||||||||||||||||||||||||||||